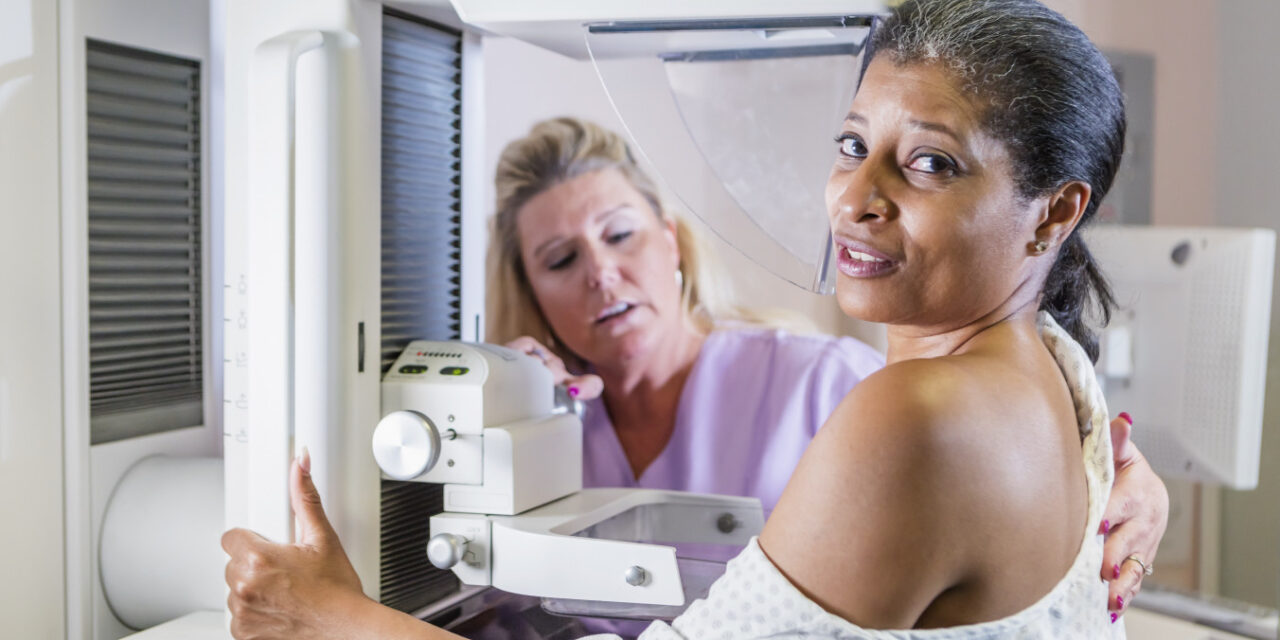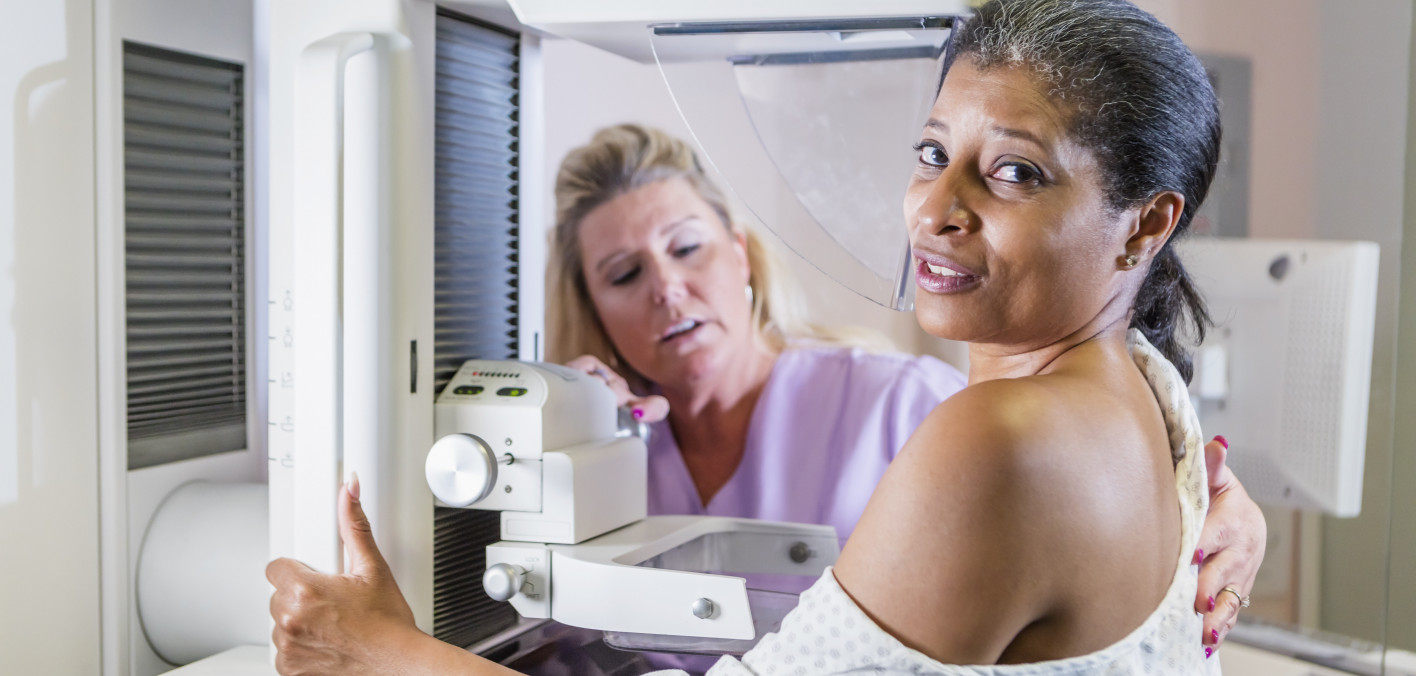
Black women have disproportionately higher rates of breast cancer compared with white women, yet many experience barriers to annual screening mammograms, according to new research published in Medical Research Archives.
Breast cancer is the leading cause of cancer-related deaths in Black women, according to the American Cancer Society. What’s more, Black are more likely to be diagnosed with triple-negative breast cancer (a rare and aggressive type) at younger ages, underscoring the importance of mammography screening and reducing barriers to care.
Researchers from Florida Atlantic University (FAU) conducted a retrospective study in a sample of Black women and looked at mammography screening frequency, perceived benefits and barriers to screening, and beliefs about breast cancer, according to an FAU article.
The study showed “suboptimal utilization” of annual mammograms among low-income Black women. About half reported having annual mammograms, while the remaining women reported having mammograms every two to three years. Some never had a mammogram despite being age 40 or older.
About 67% of women reported that it is “very unlikely” that they will get breast cancer in the next five years. Similarly, 60% thought it is “very unlikely” they will get breast cancer in their lifetime. This contrasts sharply with the fact that many women in the study perceived mammograms to be beneficial and 80% believed that “if breast cancer is found early, it’s likely that the cancer can be successfully treated.” What’s more, 90% agreed that “having a mammogram could help find breast cancer when it is first getting started,” according to FAU.
“Our findings suggest that Black women actually see the benefits of having an annual mammogram; however, some perceived and actual barriers may be preventing these women from obtaining screening mammograms at the appropriate age,” senior author Tarsha Jones, PhD, an assistant professor at FAU’s College of Nursing, told FAU.
Barriers reported in the study included: “getting a mammogram would be inconvenient for me,” “getting a mammogram could cause breast cancer,” “other health problems would keep me from having a mammogram” and “not being able to afford a mammogram would keep me from having one.” Authors note that people living in poverty often lack education about their health as well as access to resources needed to maintain their well-being.
“Living in poverty is a substantial risk factor for poor health outcomes because women who are poor do not have discretionary incomes to use as co-pays for health care services,” Jones said. “This demonstrates the importance of providing these women with free lifesaving mammograms.”