Mounting evidence shows that more young adults are experiencing heart problems compared to decades past, and that worsening lifestyle habits—namely, poor diet and lack of exercise—are to blame. And some research suggests that COVID infections are adding insult to injury.
Perhaps the most alarming trend is that, despite declines among older adults, the proportion of heart attacks among younger adults is increasing across the globe—which many doctors who spoke to National Geographic consider a public health emergency. (Young adults are loosely defined as those between 20 to 50 years old.)
Recent events have underscored these concerns. In late July, 18-year-old Bronny James, the oldest son of NBA star LeBron James, collapsed after going into cardiac arrest during basketball practice at the University of Southern California. (He has since been discharged after a short hospital stay.)
Cardiac arrest is not the same as a heart attack—but the event, and several others like it, raises questions more broadly about cardiovascular health and young people.
(It’s not just heart attacks. Colon cancer is rising among young adults.)
“Young individuals are not immune from cardiac arrest or heart attack, yet many think that this is still a disease of older folks,” sas Ron Blankstein, senior preventive cardiologist at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School in Boston. “But the really important thing for young individuals to know is that cardiovascular disease, for the most part, can be prevented if you take the right steps.”
Heart attacks on the rise in younger adults
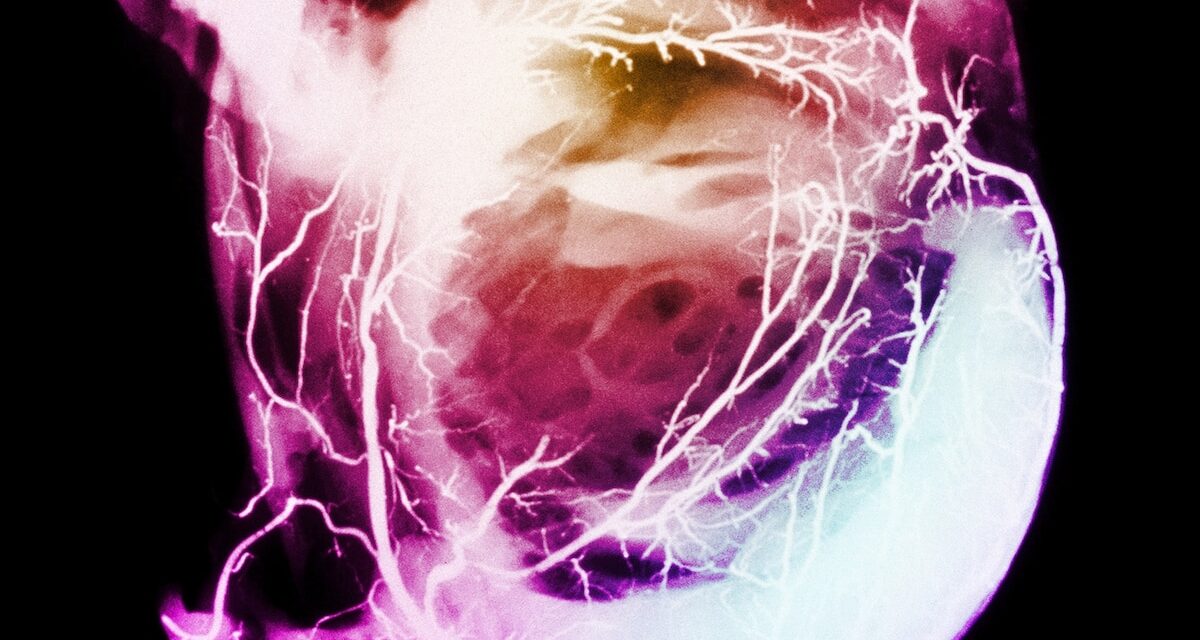
Cardiac arrest, which Bronny James suffered, occurs when the heart experiences an electrical malfunction and suddenly stops beating. This is different from a heart attack, which happens when blood flow into the heart is partially or completely blocked.
Because cardiac arrest can be caused by several conditions—like cardiomyopathy (thickened heart muscle), heart failure, arrhythmias (irregular heartbeat), and yes, heart attacks—it’s difficult for doctors to study and determine whether it’s becoming more common in young adults.
But research does show that heart attacks, also called myocardial infarctions, are on the rise in younger people. Common symptoms include chest pain or discomfort; pain that radiates into the jaw, neck, back or arms; shortness of breath; and feeling weak or faint.
A study of more than 2,000 young adults admitted for heart attack between 2000 and 2016 in two U.S. hospitals found that 1 in 5 were 40 years old or younger—and that the proportion of this group has been increasing by 2 percent each year for the last decade.
The study, published in 2019 in the American Journal of Medicine, also found that people ages 40 or younger who have had a heart attack are just as likely as older adults to die from another heart attack, stroke, or other reason.
In fact, increases in heart disease among younger adults in 2020 and 2021 are responsible for more than 4 percent of the most recent declines in life expectancy in the U.S., according to an editorial published in March in JAMA Network.
Who is most at risk?
The problem isn’t uniquely American. Research shows that adults in Pakistan and India, for example, are also experiencing heart attacks at younger ages. “Cardiovascular disease doesn’t know international boundaries,” Blankstein said, “and neither do the risk factors.”
(This doctor upended everything we knew about the human heart.)
And though heart attacks typically strike men more often than women, recent studies have suggested that more younger women are experiencing heart attacks compared to younger men—and that their outcomes are worse.
A 2018 investigation published in the journal Circulation found that the overall proportion of heart attack hospitalizations among people ages 35 to 54 increased from 27 percent in 1995-99 to 32 percent in 2010-14. The largest increase occurred in young women (21 percent to 31 percent) compared to young men (30 percent to 33 percent).
The young women in the study were more often Black and had a history of high blood pressure, diabetes, chronic kidney disease, and prior stroke.
Studies have found that clinicians are more likely to dismiss symptoms and underdiagnose certain risk factors in women, and are less likely to prescribe them medications to help manage their risks.
What are the biggest risk factors?
The majority of research shows that more people, particularly those of diverse racial and ethnic backgrounds, are developing risk factors for heart disease at younger ages—and that most of the young, seemingly healthy people who have a heart attack almost always have at least one underlying condition.
The biggest risk factors are high blood pressure, diabetes, high cholesterol, and obesity, all of which can clog and damage the arteries and blood vessels that carry oxygen-rich blood to the heart.
While some of these conditions may be genetic, more often they’re brought on by years of unhealthy habits like poor diet and a sedentary lifestyle that typically begin early in childhood, says Eugene Yang, a preventive cardiologist and chair of the American College of Cardiology Prevention of Cardiovascular Diseases Council.
COVID, on the other hand, appears to have a more immediate impact on cardiovascular health. A 2022 study published in the Journal of Medical Virology found that heart attack deaths increased by 14 percent within the first year of the pandemic. The greatest increase was found among adults aged 25 to 44.
(How COVID-19 harms the heart.)
COVID is known to activate inflammatory responses in the body and make blood thicker and stickier, Yang said, which can make infected people more susceptible to blood clots that can clog arteries and lead to heart attack. However, it’s still not clear why younger adults appear to be more vulnerable to COVID’s cardiovascular complications.
Other factors like tobacco, cocaine, marijuana, and alcohol use have been associated with increased risks of heart attack in younger adults too.
Young adults aren’t aware of their risks
Yet, most young adults aren’t concerned. A survey conducted in January by The Ohio State University Wexner Medical Center found that 47 percent of people under age 45 don’t think they’re at risk for heart disease; a third of all adults surveyed said they wouldn’t confidently know whether they were having a heart attack.
Similarly, just half of 3,500 younger adults who had significant risk factors believed they were at risk for heart disease before their heart attack occurred; even fewer reported that their doctors told them they were at risk, especially women.
Getting younger adults to care about heart health is a unique challenge, experts say; they’re busy building families and careers and are the least likely age group to have health insurance.
But it’s not all their fault. The health care system isn’t designed to effectively evaluate and treat younger adults with heart disease, Blankstein said, fueling a bias among clinicians that younger patients are at low risk.
The most widely used “risk calculator” developed by the American Heart Association, for example, only assesses risks for those ages 40-75.
Further, most young adults who had a heart attack would not have been eligible for cholesterol treatment under current guidelines before their heart attack occurred; women face even lower eligibility compared with men, despite similar risk factors.
How to reduce risks of heart attack
Early prevention is key. The longer you live with risk factors, the greater your chances of developing heart disease and experiencing worse outcomes later in life, especially if left untreated.
“Take a good look at your risk factors,” says Mariell Jessup, chief science and medical officer with the AHA, “and then develop a plan about how you can tackle one or more of those.”
(The real COVID-19 heart risk for kids is an infection—not the vaccine.)
The AHA recommends following “Life’s Essential 8”: key measures that, if practiced, can improve and maintain your cardiovascular health. These include a healthy diet, regular physical activity, no tobacco smoking, and sufficient sleep, as well as managing your weight, cholesterol, blood sugar, and blood pressure.
“Young adulthood is a phenomenal opportunity for prevention of cardiovascular disease, which goes hand in hand with overall health,” says John Wilkins, associate professor of medicine in cardiology at the Northwestern University Feinberg School of Medicine. “The better job we can do at getting young adults at these optimal levels, the greater chance they have at a longer health span.”