August 15, 2023
2 min read
Source/Disclosures
Disclosures:
NIH and NHLBI funded this study. Suen reports no relevant financial disclosures.
Key takeaways:
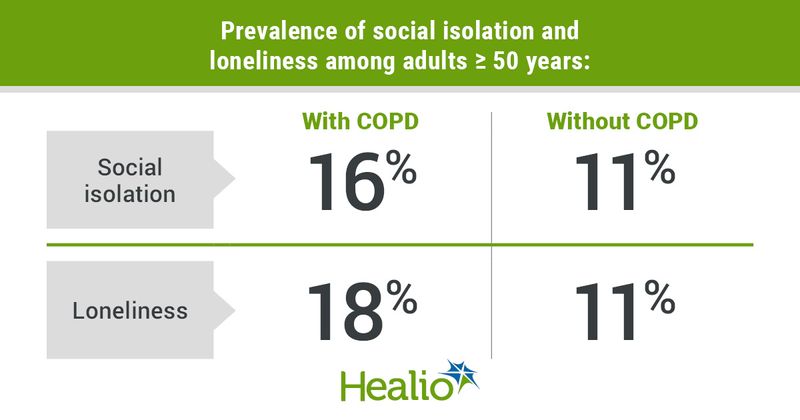
- More adults with vs. without COPD experienced social isolation and loneliness.
- Depression and at least one activity of daily living difficulty in COPD were linked to social isolation and loneliness.
Among adults aged 50 years and older, those with COPD experienced social isolation and loneliness more frequently than those without COPD, according to results published in Annals of the American Thoracic Society.

Angela O. Suen
“Our study question was informed by our clinical experience and so we were not surprised to learn that nearly one in five adults with COPD experience social isolation and loneliness,” Angela O. Suen, MD, pulmonary and critical care fellow in the division of pulmonary, critical care, allergy and sleep medicine at the University of California, San Francisco, told Healio.
In a cross-sectional study, Suen and colleagues evaluated 10,384 adults (mean age, 68 years; 54% women; 10% Black) aged 50 years or older from the Health and Retirement Study to determine the prevalence of social isolation and loneliness among those with COPD, as well as what factors are linked to these outcomes through multivariable logistic regression.
Researchers used the UCLA 3-item Loneliness Scale to determine loneliness and a 9-item scale to measure social isolation that assessed household contacts, social network interaction and community engagement.
Of the total cohort, 1,100 adults (11%) had self-reported COPD and191 (2%) had self-reported COPD on supplemental oxygen. The remaining individuals (n = 9,284) did not have COPD.
Using the scales outlined above, social isolation and loneliness were each observed in 12% of the total cohort, and 3% of patients presented with both.
Among the three groups of adults, social isolation was most prevalent in patients with COPD on oxygen (20%), followed by patients with COPD (16%) and adults without COPD (11%) in a model adjusted for age, sex, race/ethnicity, marital status and net worth (P < .05). This same pattern was found when assessing loneliness, with the most frequent occurrence of this outcome in patients with COPD on oxygen (22%), followed by patients with COPD (18%) and adults without COPD (11%), according to researchers (P < .001).
When evaluating social isolation and loneliness in patients with COPD, researchers observed several demographic and clinical characteristics linked to each outcome, with most factors differing between groups.
Social isolation in COPD was significantly linked to male sex (22% vs. women, 13%), non-Hispanic white ethnicity (19% vs. Black, 7%), a net worth of less than $6,000 (32% vs. $6,001-$81,000, 28% vs. $81,001-$239,000, 10%), depression on the modified Center of Epidemiological Studies-Depression (CES-D) scale (24% vs. no depression, 14%), having at least one activity of daily living difficulty (22% vs. no difficulty, 14%) and current smoking status (24% vs. never smoking status, 13%), according to researchers.
For loneliness in COPD, researchers observed that this was significantly linked to the age range of 50 to 64 years (22% vs. 75-84 years, 12%), single marital status (32% vs. married, 12%), depression on the CES-D scale (36% vs. no depression, 13%), having at least one activity of daily living difficulty (29% vs. no difficulty, 15%), a diagnosis of diabetes (26% vs. no diabetes, 17%) and a diagnosis of heart disease (23% vs. no heart disease, 17%).
“We hope that clinicians will consider screening for social isolation and loneliness and consider how isolated and lonely adults may experience unique challenges to obtaining medical care,” Suen told Healio.
For more information:
Angela O. Suen, MD, can be reached at angela.suen@ucsf.edu.