JenkoAtaman/AdobeStock

ADAA Partner
There are significantly larger rates of maternal mortality in the peri- and postpartum period in the United States compared with other countries across the world. The US is considered a first-world country, with a systemic prioritization placed on access and utilization of health care. However, mortality rates are 10 times that of similar first world countries. Out of every 100,000 live births, approximately 33 lead to maternal death in the US. This is in comparison to other first-world countries such as Japan or Australia, where deaths are 2 to 3 per 100,000 live births.1
Figure. Peri/postpartum Maternal Mortality Rates by Year and Race
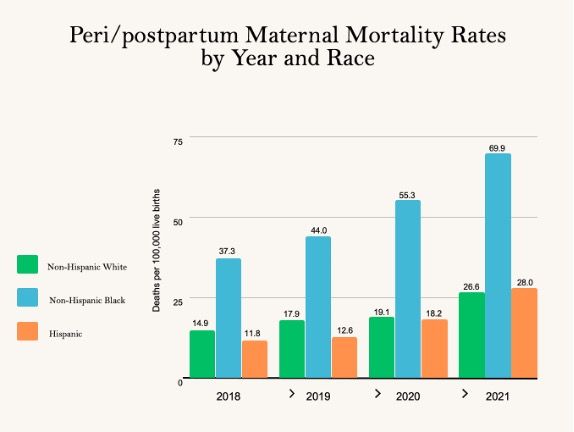
When separating out maternal mortality rates by race in the year 2021, Black women in the US experienced a far worse outcome. Maternal mortality rates were 70 in 100,000 live births. Comparatively, in white women, approximately 27 out of 100,000 live births resulted in maternal mortality.1 Preliminary data from 2022 indicate an across-the-board drop to pre-COVID-19-pandemic levels, underlying the role the pandemic played in access to adequate health care.2 See the Figure for peri/postpartum mortality rates for Black compared to white women through years 2018-2021.
At present, there are no dismantling studies examining the specific variables that contribute to the high rates of mortality in peri-and postpartum Black women. Several variables have been examined (eg, socioeconomic status, level of education/career status, access to health care, social support system, advocacy efforts, pre- or concurrent levels of medical and mental health comorbidities) and none of these alone were found to be the contributory variable.3 A Black woman with a high-level career, level of notoriety, and a higher socioeconomic status, is still at the same risk of mortality as a Black woman who does not fall within these categories. The abovementioned variables appear to be under a larger umbrella of “pervasive systemic racism” that most researchers and clinicians hypothesize to be the causal factor of high levels of mortality in peri- and postpartum Black women in the US.
Mental health comorbidities and treatment participation in Black peri- and postpartum women are some of the most important variables when considering mortality. The presence of undiagnosed and untreated anxiety and depression can influence access to and proper health care (eg, efficiently address biological comorbidities such as high blood pressure), impact infant care and wellness, and access to building effective social support systems. In the US, studies have found that the rates of peri-and postpartum depression and anxiety do not differ between Black and white women. During the peri- and postpartum period, the diagnostic rates of anxiety and depression are between 10 and 33%.4-6 Although studies show anxiety and depression rates do not differ in white vs Black peri- and postpartum women, Black women are 3 times less likely to report their symptoms and seek out evidence-based care.4,5 Thus, the rates for Black peri- and postpartum women are likely higher than studies have indicated due to low levels of reporting. While mental health may be one piece in a larger puzzle, it remains a very important one. It is comingled with the several variables listed above and is a contributing factor when considering mortality rates.
The American College for Obstetrics and Gynecologists recommends, across race, screening for anxiety and depression at least once during the peri-natal period, “closer monitoring” for those with a history of anxiety and depression, and at the one-time 6- to 8-week postpartum check-up appointment.7 Juxtapose this with evidence-based mental health clinicians, who more routinely use screening measures (weekly, if not biweekly) and have access to their patients frequently enough to follow through on early detection. The Edinburg Postnatal Depression Scale8 or Beck Anxiety/Depression Inventories9,10 are the most common measures used to detect clinical anxiety and depression in peri- and postpartum women. However, while even they have good psychometric properties, they are not sensitive to cultural and race differences in women specific to the peri- and postpartum period. After the 6- to 8-week postpartum appointment, care of the patient typically transfers back to the primary care physician. During this interval of time, the paucity of continuous care, especially when patients may experience active depression and/or anxiety, is cause for concern for self-advocacy and commitment to care. Some researchers have found there are disproportionate levels of access to and active engagement in treatment across Black postpartum women with depression.11 White postpartum women were 2 times as likely, even if actively symptomatic, to successfully initiate mental health care.11 Interestingly, Black women have been found to prefer psychotherapy over psychotropic medications,12-14 emphasizing the importance of access to mental health care prior to and after birth.
Medical and mental health comorbidities in Black women during the peri- and postpartum stage can influence the experience and outcome of the birthing and postpartum recovery process. The intertwined nature of pre-existing and/or concurrent anxiety and/or depression and medical comorbidities during the pregnancy, birth, and recovery process is individual and complicated by systemic racism underlying decades-old medical systems.
Case Example
“Tara” (identifying information and situation changed to protect patient confidentiality), a 35-year-old Black woman resided in Upper East Side of New York City. She had been married to her husband, Benny, for 10 years. They had gone through several rounds of IVF to successfully conceive and carry a baby to term. She had been diagnosed with major depressive disorder and generalized anxiety during her IVF process and remained symptomatic (seeing a psychologist), but choosing to remain unmedicated during her pregnancy. She was a pediatrician and well-versed in medical language and how to advocate for herself. At her 38-week appointment, her OB/GYN, with permission, broke her water, as Tara was dilated and complaining of severe back pain, suspected to be labor pains. Her blood pressure was borderline high (130 systolic/88 diastolic), but her OBGYN reported that was to be expected undergoing labor pains at now almost 4 cm dilated. Tara had a very smooth natural vaginal delivery and reported to her husband that she did not expect her first birth go so well.
Twenty-four hours after delivery, Tara woke up in a sweat and reported that she did not “feel well.” Her nurse came in and took her temperature, noticing it was barely above normal at 99.9 oF. Tara reported her pain was at a level of a “6” on a scale from 0-10. The nurse asked Tara and her husband about any pre-existing conditions and they reported that she was medically healthy, and had been diagnosed with depression and anxiety. The nurse ordered acetaminophen for Tara and told her she would be back in 2 hours to check on her and to get some rest. Benny reported that Tara looked better after 30 minutes. Tara awoke 1 hour later in pain. The nurse came in and noticed Tara had passed a large blood clot (can be part of the normal process of expelling birthing remains after a vaginal birth). She said that Tara would be fine and that she would order a narcotic pain killer. Tara’s pain subsided after being given the pain killer and while she was asleep the nurse reported to her husband that “some women just cannot handle the pain of childbirth, especially when they have a low tolerance for discomfort being diagnosed with anxiety and depression.”
After being discharged from the hospital, Tara continued to experience high levels of generalized pain. She called her OB/GYN and was encouraged to take more narcotics. Two to 3 days after taking narcotics, Tara’s pain continued. Her husband called an ambulance. Tara coded and passed away en route to the emergency room.
Autopsy results revealed Tara had been suffering from eclampsia that had gone undiagnosed, as her blood pressure clinically elevated into dangerous levels within days after her discharge from the hospital. Her physical complaints were misinterpreted as an anxious reaction to her birthing process and were not diagnosed and treated properly.
Improved Avenues for Care and Future Research
Upon reflection and examination of Tara’s care, it is noticeable there were several issues consisting of lack of patient advocacy, miscommunication among medical professionals and with the patient, disregard and/or the misinterpretation of symptoms experienced by the patient, minimally adequate medical and mental health care, and concerns of micro-aggressions and overt racism. If these issues had been sufficiently addressed, it may had resulted in Tara’s survival, rather than her unnecessary death.
Currently, several community-based programs have been developed to increase positive birthing outcomes and decrease medical and mental health comorbidities in Black peri-and postpartum women. Prevention programs, such as the Milwaukee Birthing Project, employed a “life course perspective” including building support systems and skills aimed to reduce a cumulative life stressor response (systemic racism) thought to contribute to both infant and maternal mortality rates.15 Each mother was paired with a “big sister” to communicate with on a biweekly basis with goals such as improving prenatal care, birth outcomes, increasing social network access, and more. These were part of a larger 12-point plan to reduce the disparity in the Black-white birthing outcome. Results were promising, indicating improved birth outcomes compared with a control group, but the data was limited due to poor follow-up with participants.15
Table. 5 Areas of Well-Being for Health Care Providers to Address16

The UNC Collaborative Center for Maternal and Infant Health has sought to recommend a more comprehensive approach. Depression in the peri- and postpartum period has been found to have an intergenerational aspect, where adults who have been neglected tend to pass on the neglect to the care of their infant.16 Therefore, in addition to the recommendation of evidence-based mental health treatment (eg, cognitive-behavioral treatment for anxiety and depression), the 4th trimester project recommends health care providers address 5 other areas of well-being (Table).16 This research has found that postpartum care (termed 4th trimester), should be designed for a Black woman’s individual needs and constraints, should be implemented prior to birth; improve upon patient-provider communication; focus on retention and activation of information received from the provider to the patient; and should be empathic, culturally-sensitive, and aware of systemic racism underlying the US health care system.17,18
These programs have called for a more holistic approach to peri- and postpartum health care in Black women. Assessing and treating mental health concerns, such as anxiety and depression, is vital in peri- and postpartum Black women, but it is also not the entire clinical package that is needed. One of the major obstacles to following through with a more holistic approach is continuity of care. While health care providers have been found to provide helpful recommendations, the onus of responsibility for follow through on the recommendations relies solely on the patient, who may not have the financial, social, mental, physical, or logistic support to successfully implement adequate care. Providers may fall victim themselves to perpetuating an ineffective health care system, not knowing the limitations of the patients themselves.17 Larger changes in US government policy and grant allocation, as well as peri- and postpartum education of providers (eg, effective and empathic communication systems with marginalized groups and recognizing the role of systemic racism, etc) and patients (eg, education in mental and physical health of the mother and infant at different stages in peri- and postpartum care, etc), are needed to drastically improve peri- and postpartum mortality (and morbidity) of marginalized groups, especially that of Black women.
Dr Kaplan is a clinical psychologist and director of the Washington Anxiety Center of Capitol Hill. Dr Dumessa is a clinical psychologist at the Washington Anxiety Center of Capitol Hill.Ms Ruiz is research assistant and graduate student at the Washington Anxiety Center of Capitol Hill and the Catholic University of America.
References
1. Hoyert DL. Maternal mortality rates in the United States, 2021. Centers for Disease Control and Prevention, National Center for Health Statistics. 2023. Accessed July 20, 2023. https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2021/maternal-mortality-rates-2021.pdf.
2. Provisional maternal deaths. Centers for Disease Control and Prevention, National Center for Health Statistics. July 12, 2023. Accessed July 20, 2023. https://www.cdc.gov/nchs/nvss/vsrr/provisional-maternal-deaths.htm.
3. Gavin NI, Gaynes BN, Lohr KN, et al. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5):1071-1083.
4. Kozhimannil KB, Trinacty CM, Busch AB, et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011;62(6):619-625.
5. Dagher RK, Pérez-Stable EJ, James RS. Socioeconomic and racial/ethnic disparities in postpartum consultation for mental health concerns among US mothers. Arch Womens Ment Health. 2021;24(5):781-791.
6. Ponting C, Urizar GG Jr, Dunkel Schetter C. Psychological interventions for prenatal anxiety in Latinas and Black women: a scoping review and recommendations. Front Psychiatry. 2022;13:820343.
7. ACOG Statement on Depression Screening. American College of Obstetricians and Gynecologists. January 26, 2016. Accessed July 20, 2023. https://www.acog.org/news/news-releases/2016/01/acog-statement-on-depression-screening.
8. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-786.
9. Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561-571.
10. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893-897.
11. Kozhimannil KB, Trinacty CM, Busch AB, et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011;62(6):619-625.
12. Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003;41(4):479-489.
13. Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323-331.
14. Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. 2009;36(1):60-69.
15. Mkandawire-Valhmu L, Lathen L, Baisch MJ, et al. Enhancing healthier birth outcomes by creating supportive spaces for pregnant African American women living in Milwaukee. Matern Child Health J. 2018;22(12):1797-1804.
16. Chamberlain C, Gee G, Harfield S, et al. Parenting after a history of childhood maltreatment: a scoping review and map of evidence in the perinatal period. PLoS One. 2019;14(3):e0213460.
17. Verbiest S, Tully K, Simpson M, Stuebe A. Elevating mothers’ voices: recommendations for improved patient-centered postpartum care. J Behav Med. 2018;41(5):577-590.
18. Timilsina S, Dhakal R. Knowledge on postnatal care among postnatal mothers. Saudi Journal of Medical and Pharmaceutical Sciences. 2015;1(4):87-92.