- Andrew S Oseran, postdoctoral fellow1 2,
- Yang Song, statistician1,
- Jiaman Xu, statistician1,
- Issa J Dahabreh, associate professor1 3,
- Rishi K Wadhera, assistant professor1 4,
- James A de Lemos, professor5,
- Sandeep R Das, professor5,
- Tianyu Sun, statistician1,
- Robert W Yeh, professor14,
- Dhruv S Kazi, associate professor14
- 1Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center, Boston, MA 02215, USA
- 2Division of Cardiology, Massachusetts General Hospital and Harvard Medical School, Boston, MA, USA
- 3CAUSALab, Department of Epidemiology, and Department of Biostatistics, Harvard T.H. Chan School of Public Health, Boston, MA, USA
- 4Division of Cardiology, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, MA, USA
- 5Division of Cardiology, University of Texas Southwestern Medical Center, Dallas, TX, USA
- Correspondence to: D S Kazi dkazi{at}bidmc.harvard.edu (or @kardiologykazi on Twitter)
- Accepted 7 July 2023
Abstract
Objectives To characterize the long term risk of death and hospital readmission after an index admission with covid-19 among Medicare fee-for-service beneficiaries, and to compare these outcomes with historical control patients admitted to hospital with influenza.
Design Retrospective cohort study.
Setting United States.
Participants 883 394 Medicare fee-for-service beneficiaries age ≥65 years discharged alive after an index hospital admission with covid-19 between 1 March 2020 and 31 August 2022, compared with 56 409 historical controls discharged alive after a hospital admission with influenza between 1 March 2018 and 31 August 2019. Weighting methods were used to account for differences in observed characteristics.
Main outcome measures All cause death within 180 days of discharge. Secondary outcomes included first all cause readmission and a composite of death or readmission within 180 days.
Results The covid-19 cohort compared with the influenza cohort was younger (77.9 v 78.9 years, standardized mean difference −0.12) and had a lower proportion of women (51.7% v 57.3%, −0.11). Both groups had a similar proportion of black beneficiaries (10.3% v 8.1%, 0.07) and beneficiaries with dual Medicaid-Medicare eligibility status (20.1% v 19.2%; 0.02). The covid-19 cohort had a lower comorbidity burden, including atrial fibrillation (24.3% v 29.5%, −0.12), heart failure (43.4% v 49.9%, −0.13), and chronic obstructive pulmonary disease (39.2% v 52.9%, −0.27). After weighting, the covid-19 cohort had a higher risk (ie, cumulative incidence) of all cause death at 30 days (10.9% v 3.9%; standardized risk difference 7.0%, 95% confidence interval 6.8% to 7.2%), 90 days (15.5% v 7.1%; 8.4%, 8.2% to 8.7%), and 180 days (19.1% v 10.5%; 8.6%, 8.3% to 8.9%) compared with the influenza cohort. The covid-19 cohort also experienced a higher risk of hospital readmission at 30 days (16.0% v 11.2%; 4.9%, 4.6% to 5.1%) and 90 days (24.1% v 21.3%; 2.8%, 2.5% to 3.2%) but a similar risk at 180 days (30.6% v 30.6%;–0.1%, −0.5% to 0.3%). Over the study period, the 30 day risk of death for patients discharged after a covid-19 admission decreased from 17.9% to 7.2%.
Conclusions Medicare beneficiaries who were discharged alive after a covid-19 hospital admission had a higher post-discharge risk of death compared with historical influenza controls; this difference, however, was concentrated in the early post-discharge period. The risk of death for patients discharged after a covid-19 related hospital admission substantially declined over the course of the pandemic.
Introduction
The covid-19 pandemic has resulted in more than 1.1 million deaths in the United States as of June 2023, with most of this burden concentrated among Medicare beneficiaries.12 Older adults and individuals with a high comorbidity burden are at greater risk of adverse outcomes and have been a major focus of clinical interventions and public health measures.13 Although the acute manifestations of covid-19 and associated short term outcomes have been well studied in the Medicare population, longer term outcomes in elderly adults have been less well defined.
Patients who require covid-19 related hospital admission are a large population with distinct clinical and public health considerations. They have a greater comorbidity burden, more severe initial disease, and worse short term outcomes compared with patients with an asymptomatic or mildly symptomatic clinical course, and they may be more vulnerable to late complications of infection.4 Better understanding of the post-discharge risk of adverse health outcomes (eg, death) may help tailor preventive strategies, while knowledge of post-discharge healthcare utilization such as readmission may facilitate resource allocation in the context of intermittent surges of covid-19 or during future pandemics.56 Moreover, given advances in therapeutics, growing population level immunity, and changes in the characteristics of SARS-CoV-2, such as transmissibility and virulence, understanding how outcomes changed over the course of the pandemic is critical to informing the ongoing management of individuals recovering from covid-19 and future public health interventions.
In this study, we used data on Medicare fee-for-service claims to answer three related questions. Firstly, what are the clinical and sociodemographic characteristics of Medicare fee-for-service beneficiaries aged ≥65 years who were discharged alive from a hospital admission with covid-19? Secondly, what is the long term risk of death and readmission among people who were discharged alive from a covid-19 hospital admission, and how has this changed over time? Thirdly, to help contextualize our findings, how does the risk of death and readmission among people discharged alive from a covid-19 hospital admission compare with a historical control of patients who were admitted to hospital with influenza?
Methods
Our study adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies.7 All data management and analyses were performed through the CMS Virtual Research Data Center and were conducted using SAS version 9.4 (SAS Institute, Cary, NC).8
Data sources and study population
We used 100% Medicare fee-for-service hospital inpatient claims to identify hospital admissions at short term acute care hospitals between 1 March 2020 and 31 August 2022 with a principal or secondary discharge diagnosis of covid-19.9 Admissions with covid-19 were identified using international classification of diseases, clinical modification (ICD-10-CM), 10th revision, codes U07.1 (covid-19), B97.29 (other coronavirus as the cause of disease classified elsewhere), and J12.82 (pneumonia due to covid-19).10 In addition, we identified a historical control cohort of Medicare fee-for-service beneficiaries admitted to hospital with influenza between 1 March 2018 and 31 August 2019, using ICD-10-CM codes utilized in previous studies (see supplement table 1).11 We chose historical rather than contemporaneous controls given the substantial epidemiological changes in influenza rates during the covid-19 pandemic as a result of social and clinical practices.12 These years were chosen to avoid overlapping study periods. To account for the seasonality of respiratory viruses, the study periods of our two cohorts (covid-19 and influenza) began and ended in the same calendar month.
We included Medicare beneficiaries aged ≥65 years who were enrolled in Medicare fee-for-service for at least one year before the index admission (to adequately capture baseline comorbidities) and were alive at discharge from the index hospital admission (see supplement figure 1). As in previous work with Medicare claims, inpatient hospital claims separated by one day or less were treated as a single episode of care.13 Baseline patient personal and monthly Medicare enrollment data were identified using the Medicare Beneficiary Summary Files.14 Race/ethnicity was designated as the three fixed categories of white people, black people, or other. Race/ethnicity was included as a covariate in the analysis because it is associated with the risk of death among patients with covid-19.2 Patient comorbidities were ascertained using the CMS Chronic Conditions Data Warehouse, which identifies the presence of 30 chronic conditions.15 Characteristics of discharging hospitals were obtained from the 2020 American Hospital Association annual survey.16
Outcomes
The primary outcome was death from any cause within 180 days of discharge from the index hospital admission. Secondary outcomes included first readmission for any cause (accounting for the competing risk of death), a composite of all cause death or readmission within 180 days of discharge, as well as the primary reason for all readmissions within 180 days of discharge.
Statistical analysis
We first examined baseline patient characteristics (age, sex, race, geographic region, dual Medicare-Medicaid eligibility status (a proxy for socioeconomic status)), clinical comorbidities, and characteristics of discharging hospitals at which both the covid-19 cohort and the influenza cohort received care (hospital size (small, medium, large), teaching status (major, minor, none)). Groups were compared using standardized mean differences, with differences greater than 0.1 or less than -0.1 considered significant.17 For both groups we calculated the crude risk (ie, cumulative incidence) of death, readmission, and a composite of death or readmission. Specifically, we applied Kaplan-Meier methods to estimate the risk of death and the composite outcome at each time point. For readmissions, we estimated risks based on the cumulative incidence function accounting for the competing event of death; P values to compare the cumulative incidence functions were calculated using the Fine-Gray method.18 Patients were censored on the last day of data availability, the last day of Medicare fee-for-service coverage, or the end of the study period, whichever came first. Finally, we examined these same outcomes among the overall cohort as well as by race (black people, white people, other) and Medicaid-Medicare dual enrollment status.
To examine changes in the risk of death over the course of the pandemic, we calculated the seven day rolling average of the estimated risk of death at 30 days, 90 days, and 180 days based on date of discharge—that is, the average estimated risk on a given calendar day and the six days previously. We plotted this rolling average of risk against time since hospital discharge using a non-parametric locally weighted smoothing method, with bandwidth parameter set to 0.1. For comparison, we created the corresponding plot for the influenza cohort.
Next, we classified the reason for readmission based on primary ICD-10 diagnosis codes, first by disease system (eg, circulatory, respiratory), consistent with the predefined ICD-10-CM code taxonomy, and then using a more specific and clinically meaningful taxonomy developed after review of the most common ICD-10-CM codes within each system (eg, cardiogenic shock).19 For readmissions with the primary diagnosis of covid-19 or influenza, we used the secondary ICD diagnosis code to classify the readmission because readmissions in the first 180 days after discharge from the index hospital admission were assumed to be unlikely to represent recurrent acute infection (covid-19, n=40 308; influenza, n=321)).20 Readmission rates were calculated per 10 000 person months and were compared between groups using a Poisson regression model.
Finally, we accounted for differences in baseline characteristics between cohorts by standardization using weighting methods, with the distribution of the covid-19 cohort as the standard.21 Specifically, we assigned a weight of 1 to patients in the covid-19 cohort and a weight equal to the inverse of the odds of membership in the influenza cohort conditional on covariates for individuals in that cohort. All of the patient personal, clinical comorbidities, and hospital level characteristics were included when estimating the odds of membership in the influenza cohort using logistic regression (see table 1). Although we had complete patient level (demographic and clinical) covariate data, a small proportion of patients (n=18 913 (2.1%) in the covid-19 cohort and n=1232 (2.2%) in the influenza cohort) were missing hospital level covariate data and were excluded from this portion of the analysis. To assess covariate balance, we compared groups after the application of weights. We then used non-parametric methods to estimate the absolute difference in the risk of death (Kaplan-Meier approach), readmission (cumulative incidence function approach), and the composite of death or readmission at 30, 90, and 180 days after discharge. We obtained 95% confidence intervals based on the standard error from 200 bootstrap samples. To better characterize whether differences in the risk of death after covid-19 related versus influenza related hospital admission changed over the course of follow-up, we estimated and plotted the time varying hazard ratio for death between 0 and 180 days of discharge.
Sensitivity analyses
We performed several sensitivity analyses. First, we defined the covid-19 and influenza cohorts using only the primary international classification of diseases discharge diagnosis field (rather than primary or secondary), thus defining a more specific patient population. This accounted for the fact that as testing became more widely available over the course of the pandemic, many hospitals began to test all patients for covid-19 at the time of admission. As a result, some patients may have been discovered to have asymptomatic SARS CoV-2 infection when admitted to hospital for other indications. Second, we excluded patients who were discharged to hospice services (n=45 405 (5.0%) in the covid-19 cohort and n=1131 (2.0%) in the influenza cohort). Third, we included patients with missing hospital level data by omitting hospital level covariates when modeling the odds of membership in the influenza cohort to estimate weights.
Patient and public involvement
No patients or members of the public were involved in the planning, design, or interpretation of the study. The study involved examination of existing claims data and therefore no participants were recruited for this analysis.
Results
Baseline characteristics
Among 1 059 060 Medicare fee-for-service beneficiaries admitted to hospital with covid-19 during the study period, 883 394 were discharged alive from the index hospital admission (16.6% had an in-hospital death) and were included in the covid-19 cohort. Among 57 947 Medicare fee-for-service beneficiaries admitted to hospital with influenza during the study period, 56 409 were discharged alive from the index hospital admission (2.7% in-hospital death) and were included in the influenza cohort as historical controls (table 1).
Characteristics of Medicare fee-for-service beneficiaries discharged alive after hospital admission with covid-19 (2020-21) or influenza (2018-19). Values are number (percentage) unless stated otherwise
The covid-19 cohort was younger (77.9 v 78.9 years; standardized mean difference −0.12) and had a lower proportion of women (51.7% v 57.3%; −0.11) compared with the influenza cohort. Both groups had a similar proportion of black beneficiaries (10.3% v 8.1%; 0.07) and beneficiaries of dual Medicaid-Medicare eligibility status (20.1% v 19.2%; 0.02). In general, the covid-19 cohort had fewer baseline comorbidities, including a lower prevalence of atrial fibrillation (24.3% v 29.5%; −0.12), heart failure (43.4% v 49.9%; −0.13), ischemic heart disease (61.6% v 66.8%; −0.11), chronic obstructive pulmonary disease (39.2% v 52.9%; −0.27), and asthma (19.6% v 27.6%; −0.19). The mean length of hospital stay was longer in the covid-19 cohort (8.6 v 5.3 days; 0.35) and fewer patients were discharged directly home (585 704 (66.3%) v 41 435 (73.5%); −0.15). The characteristics of discharging hospitals were similar between the two cohorts.
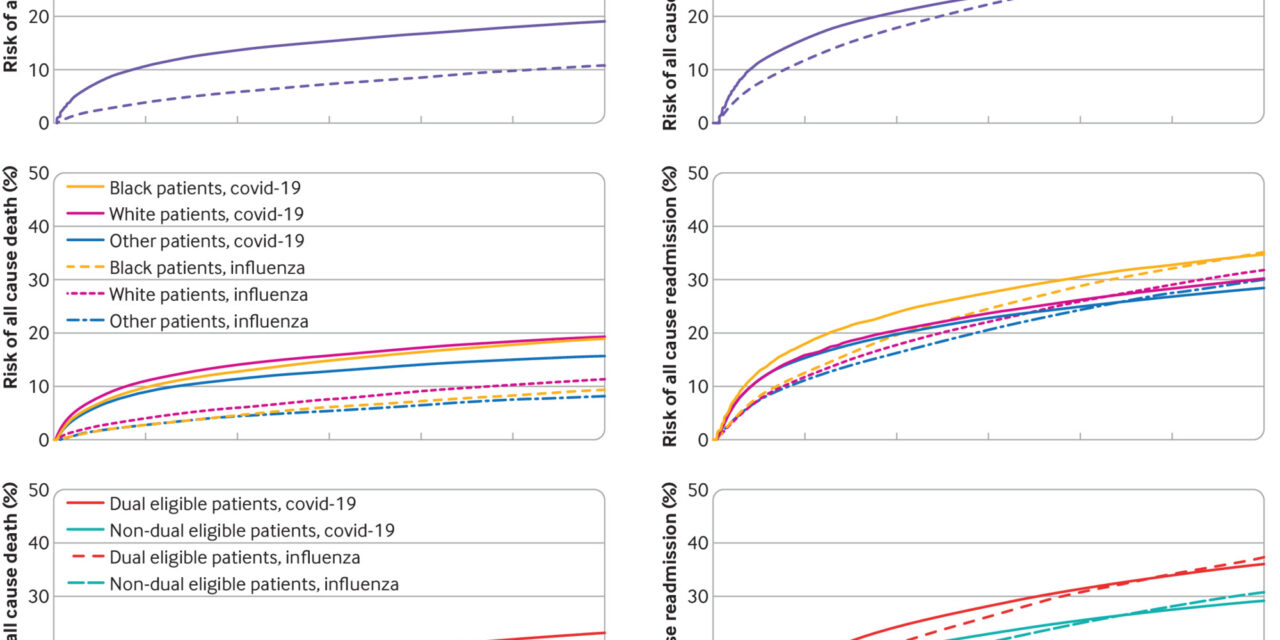
Risk of post-discharge death and readmission
In the covid-19 cohort, the risk of death was 10.9% at 30 days, 15.5% at 90 days, and 19.1% at 180 days. The risk of readmission was 16.0% at 30 days, 24.1% at 90 days, and 30.6% at 180 days (fig 1). The risk of the composite outcome of death or readmission was 21.0% at 30 days, 31.8% at 90 days, and 41.1% at 180 days (see supplement figure 2). Significant differences were found in the 180 day risk of post-discharge death and readmissions by race and socioeconomic status. The 180 day risk of death was slightly lower in black patients compared with white patients (19.0% (95% confidence interval 18.8% to 19.3%) v 19.5% (19.3% to 19.5%), P<0>v 30.2% (30.1% to 30.4%), P<0>v 18.0% (17.9% v 18.1%), P<0>v 29.2% (29.1% v 29.3%), P<0>
Risk of all cause death and readmission after live discharge from covid-19 and Influenza related hospital admission
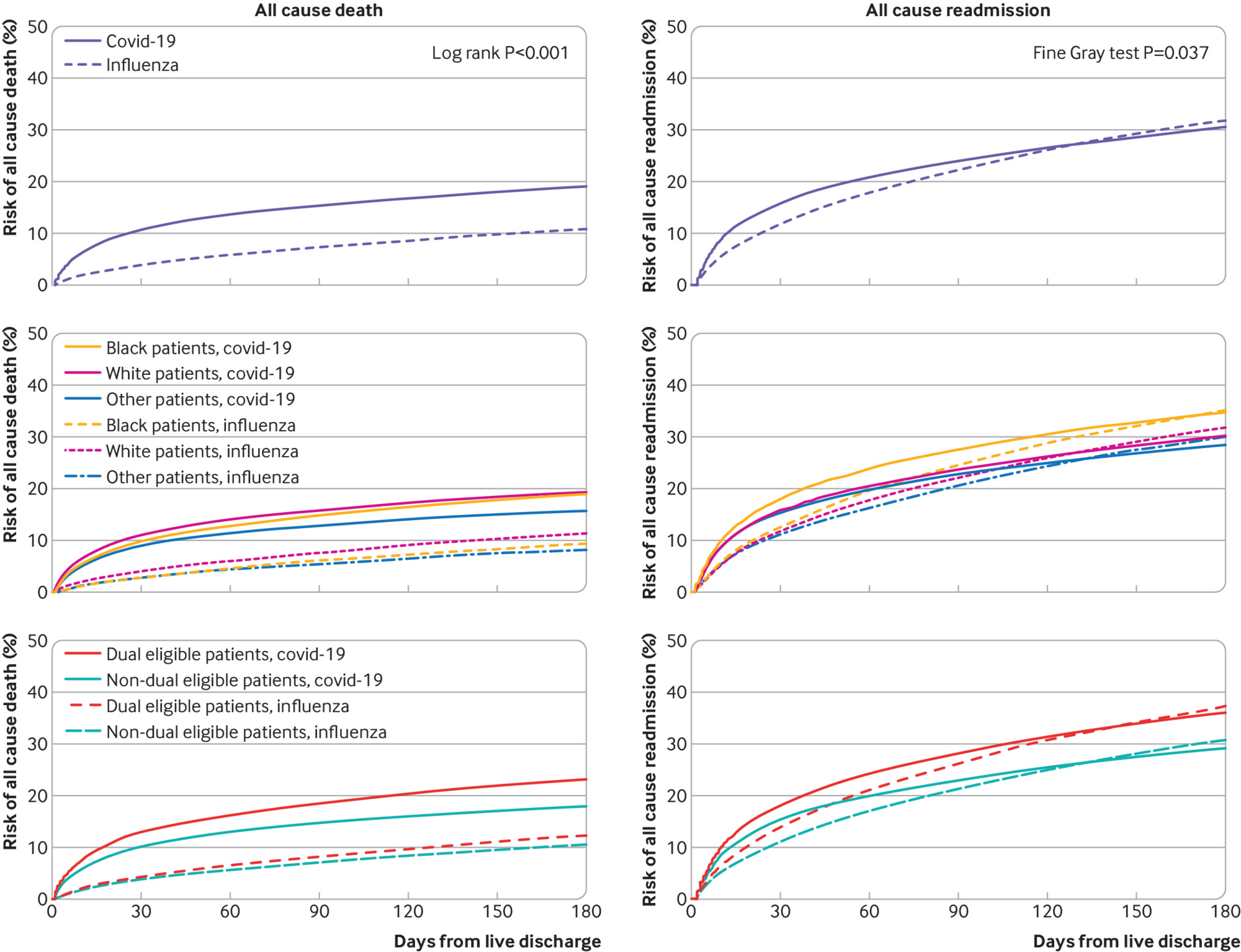
The risk of death after covid-19 related hospital admission declined over the study period but remained relatively stable after influenza related hospital admission (fig 2). The 30 day risk of death after hospital admission with covid-19 peaked at 17.9% on 1 May 2020 but decreased to 7.2% by the end of the study period.
Risk of death at 30, 90, and 180 days after discharge from covid-19 and influenza related hospital admission based on date of discharge
Primary reason for readmission
A total of 341 554 readmissions occurred within 180 days of discharge from the index covid-19 related hospital admission, corresponding to a rate of 904.4 readmissions per 10 000 person months (v 905.7 per 10 000 person months in the influenza cohort, P=0.82) (table 2). The most common reasons for readmission by system were circulatory conditions (179.1 readmissions per 10 000 person months) and respiratory conditions (174.5 readmissions per 10 000 person months). The most common primary diagnoses for readmission were sepsis (147.9 readmissions per 10 000 person months), heart failure (73.3 readmissions per 10 000 person months), and pneumonia (68.0 readmissions per 10 000 person months).
Readmission rates after covid-19 and influenza related hospital admission based on primary discharge diagnosis*
Comparison of standardized risks of post-discharge death and readmission
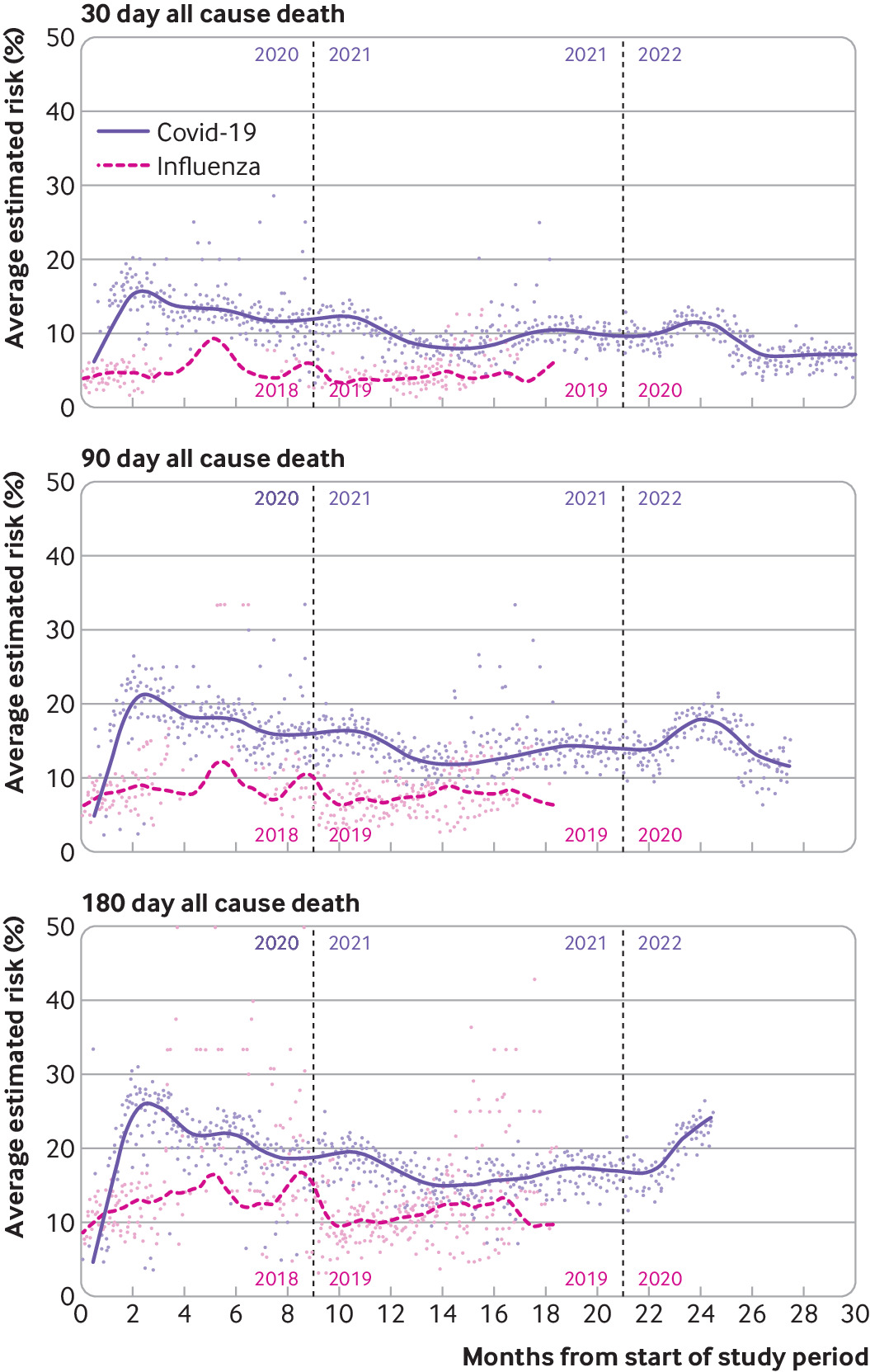
The covid-19 cohort had a higher standardized risk of all cause death at 30 days (10.9% v 3.9%; standardized risk difference 7.0%, 95% confidence interval 6.8% to 7.2%), 90 days (15.5% v 7.1%; 8.4%, 8.2% to 8.7%), and 180 days (19.1% v 10.5%; 8.6%, 8.3% to 8.9%) compared with the standardized influenza cohort. The covid-19 cohort also experienced a higher standardized risk of hospital readmission at 30 days (16.0% v 11.2%; 4.9%, 4.6% to 5.1%) and 90 days (24.1% v 21.3%; 2.8% (2.5% to 3.2%), but a similar risk at 180 days (30.6% v 30.6%;–0.1%, −0.5% to 0.3%) (fig 3). The covid-19 cohort experienced a higher risk of the composite outcome of death or readmission at 30 days (21.0% v 12.0%; 8.9%, 8.8% to 9.1%), 90 days (31.8% v 23.4%; 8.4%, 8.1% to 8.6%), and 180 days (41.1% v 35.6%; 5.7%, 5.4% to 6.0%) (see supplement figure 3). The hazard ratio for death among patients discharged after covid-19 related admission was 3.7 (95% confidence interval 3.6 to 3.8) immediately after discharge, 2.1 (2.0 to 2.1) at 30 days, and 1.04 (1.0 to 1.1) at 180 days, compared with patients discharged after an influenza admission (see supplement figure 4).
Sensitivity analyses
Findings were similar when the covid-19 and influenza cohorts were defined using primary (rather than primary and secondary) discharge diagnoses and when accounting for missing covariate data. When people with hospice discharges were excluded, the standardized risk difference between cohorts was smaller for the outcome of death but greater for the outcome of readmission, relative to the main analysis (see supplement table 4).
Discussion
This study builds on a robust literature investigating the short term clinical consequences of covid-19 and provides several important insights into longer term outcomes.222324 First, among patients who were discharged alive from a covid-19 related hospital admission, the risk of post-discharge death was nearly twice that observed in historical controls admitted to hospital with influenza, with most of the difference occurring within 30 days of discharge. Second, although readmissions after covid-19 related hospital admission were common, they were similar in frequency by 180 days to that of patients discharged alive from an influenza related hospital admission. Third, adverse post-discharge outcomes are unequally distributed in the population: black and dual eligible Medicare beneficiaries experience worse long term outcomes after hospital admission with covid-19. Fourth, long term post-discharge risk of death has declined over the course of the pandemic.
Individuals who were admitted to hospital with covid-19 and were discharged alive had a higher risk of death compared with those who were discharged alive from an influenza related hospital admission. This increased risk seems to be predominantly driven by differences within 30 days of discharge, however, potentially implicating more severe acute infection and associated short term complications. For example, patients admitted to hospital with covid-19 have been shown to be at increased risk of extrapulmonary organ dysfunction compared with those admitted to hospital with influenza.25 Although this finding may be due to differences in the biology of SARS-CoV-2 and influenza viruses, it may also reflect differences in baseline immunity between cohorts, either from previous infection or from vaccination, though we were unable to evaluate the underlying mechanism in this study. Nevertheless, the substantial in-hospital and early post-discharge risk of death associated with covid-19 in this sample exclusively of Medicare fee-for-service beneficiaries highlights the need for preventive interventions, particularly in patients at increased long term risk of adverse outcomes.
We also found that individuals who are discharged alive after hospital admission for acute covid-19 continue to have a high incidence of healthcare utilization during long term follow-up. Previous work that evaluated smaller cohorts of patients found readmission rates after covid-19 related hospital admission of nearly 9.8% at 30 days and 19.9% at 60 days.2223 We extend this work by evaluating the entire fee-for-service Medicare population and found that by 180 days, the risk of readmission exceeds 30%, with more than 340 000 readmissions in our study cohort. By 180 days, however, the overall risk of readmission among those discharged alive after covid-19 related hospital admission was similar to that after influenza related hospital admission. Although we observed readmissions across a range of primary clinical diagnoses after the covid-19 index hospital admission, including high risk of cardiovascular related hospital admissions, additional work is needed to clarify any potential biologic mechanisms between SARS-CoV-2 and other clinical diagnoses. Understanding the resources required to adequately manage the acute phase of infection as well as any downstream consequences can help plan for future surges in covid-19 cases or future pandemics.
Individuals on a low income and those from racial/ethnic minority populations have been shown to be at increased risk for adverse events associated with acute covid-19, including higher rates of infection, hospital admissions, and in-hospital death.26272829 Here we found that many of these inequalities persist among a cohort of patients who were discharged alive after the index covid-19 related hospital admission. Specifically, we observed a higher risk of both death and readmission among dual Medicare-Medicaid eligible beneficiaries, which were apparent as early as 30 days after discharge and continued to widen over the study period. Previous work has suggested that these high risk populations are more vulnerable to disruptions in healthcare access due to the pandemic (eg, inadequate outpatient follow-up), which may partially explain our findings.30 Beneficiaries with dual Medicaid-Medicare eligibility also experienced higher risk of post-discharge death. Although we observed a higher risk of readmission among black patients compared with white patients after the index covid-19 hospital admission, black patients experienced slightly lower risk of death at 180 day post-discharge. It is possible that the lack of persistent inequalities in the risk of death at 180 days among black patients is explained by an excess of short term adverse events, including death, experienced by those with the most severe disease.
The decline in the risk of post-discharge death over the study period is encouraging. The robustness of this finding in sensitivity analyses suggests that it cannot entirely be explained by shifts in coding or testing patterns over the course of the pandemic, and it is consistent with recent work performed in the United States Veterans Affairs health system.31 At least three explanations for this finding are plausible. First, major advances have been made in covid-19 treatment, including the use of steroids in the management of acute covid-19 as well as the availability of several highly effective vaccines.323334 It is possible that these interventions have resulted in less severe disease at index hospital admission and therefore discharge of an overall healthier cohort of people. Second, public health measures specifically targeting elderly and high risk patient populations, including those in nursing homes and long term care facilities, may have helped protect the most vulnerable from more recent surges in covid-19 cases.3536 Third, growing population level immunity as well as changes in the virulence of SARS-CoV-2 variants over the course of the pandemic may have contributed to the declining long term risk of post-discharge death.37 Although these findings are grounds for optimism, we did observe a transient spike in post-discharge risk of death in early 2022, corresponding to the emergence of the omicron variant, which suggests the need for continued vigilance with new variants.38
Strengths and limitations of this study
This study must be interpreted in the context of its limitations. First, we identified covid-19 and influenza admissions based on ICD-10 codes. A specific covid-19 code was implemented one month into our study period (April 2020) and was later subject to add-on payments from CMS, which may have resulted in differential coding patterns or intensity compared with historical influenza controls.1039 Second, we were unable to reliably differentiate nosocomial from community acquired covid-19 infections. However, nosocomial infections likely represent a small portion of overall covid-19 infections and therefore do not explain all of the excess morbidity and mortality observed compared with the influenza cohort.4041 Third, we did not adjust for severity of covid-19 or influenza during the index hospital admission, but instead included all patients who were admitted to hospital with that primary diagnosis during the relevant study period. This was concordant with our goal to characterize long term outcomes among those discharged alive after covid-19 related hospital admission, regardless of initial clinical course. Fourth, the clinical burden of influenza (eg, infections, deaths) varies by season; therefore, it is possible that the differences in post-discharge outcomes observed between cohorts may have been different when compared with other influenza seasons.42 Fifth, this study included Medicare beneficiaries aged ≥65 years in the US, and therefore the findings may not generalize to different populations in different settings. Sixth, the observational nature of our study design and the complex effects of the covid-19 pandemic on the US healthcare system, public policies, and individual behaviors prevent any causal interpretations of our comparison in outcomes between the covid-19 and influenza cohorts.
Conclusion
In this descriptive study of long term outcomes among individuals aged ≥65 years who were discharge alive after their index covid-19 related hospital admission, we found a high risk of death and readmission within the 180 days after discharge compared with historical influenza controls. This difference, however, was concentrated in the early post-discharge period. The risk of death after discharge from a covid-19 related admission substantially declined during the pandemic.
What is already known on this topic
-
The covid-19 pandemic has resulted in more than 1.1 million deaths in the United States as of June 2023, with most of this burden concentrated among Medicare beneficiaries
-
While the acute manifestations of covid-19 and associated short term outcomes have been well studied in this population, longer term outcomes in older adults have been less well described
What this study adds
-
In this descriptive analysis, among people aged ≥ 65 years who were discharged alive after an index covid-19 related hospital admission, a high risk of death and readmission was found within 180 days after discharge
-
Compared with historical influenza controls, those who were discharged alive after covid-19 related hospital admission had higher risk of post-discharge death; this difference, however, was concentrated in the early post-discharge period
-
The risk of death after discharge from a covid-19 related hospital admission substantially declined during the pandemic
Ethics statements
Ethical approval
This study was approved by the institutional review board of Beth Israel Deaconess Medical Center, with a waiver of informed consent for retrospective data analysis.
Data availability statement
No additional data available owing to data use agreement with the Centers for Medicare and Medicaid Services.
Footnotes
-
Contributors: RWY and DSK contributed equally as senior authors. All authors conceived and designed the study, analyzed and interpreted the data, and critically revised the manuscript for important intellectual content. RWY and DSK acquired the data. YS, JX, IJD, and TS carried out the statistical analysis. ASO, RWY, and DSK drafted the manuscript. RWY and DSK supervised the study and are the guarantors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
-
Funding: This work was supported in part by grants from the National Heart, Lung, and Blood Institute (R01HL157530) and Patient-Centered Outcomes Research Institute (PCORI) (ME-1502-27794). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
-
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from the National Heart, Lung, and Blood Institute and Patient-Centered Outcomes Research Institute. TS is currently employed by Moderna; his involvement in this project occurred while he was employed at the Richard A. and Susan F. Smith Center for Outcomes Research, before his employment at Moderna. IJD is the principal investigator of research agreement between Harvard and Sanofi on statistical methods for vaccine trials with applications to influenza, and has received consulting fees from Moderna. The other authors report no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
-
The lead authors (RWY and DSK) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained,
-
Dissemination to participants and related patient and public communities: The findings will be disseminated through academic presentations and media coverage. Since the study analyzes claims data collected during routine care, we are unable to specifically disseminate results to study participants beyond the usual channels of publication and academic presentation.
-
Provenance and peer review: Not commissioned; externally peer reviewed.