Key Points
Question
What is the natural history of disability and caregiving of persons entering long-term care facilities?
Findings
Prior to entry, almost half of nursing home (NH) entrants and one-tenth of assisted living (AL) entrants experienced a month or more of severe disability and almost all entrants had a home caregiver, but only one-third had a paid caregiver. Home caregiving was significant: the average NH and AL entrant received 27 and 18 hours of help per week; before they moved, respectively; within 2 years of entry, severe disability was present in two-thirds of AL residents, comparable to 88% in NH residents.
Meaning
This cohort study found that persons often enter NHs and ALs after months of severe disability and escalating help at home, usually from unpaid caregivers; AL residents move when less disabled, but approach levels of disability comparable to NH entrants within 2 years.
Importance
Many older persons move into long-term care facilities (LTCFs) due to disability and insufficient home caregiving options. However, the extent of disability and caregiving provided around the time of entry is unknown.
Objective
To quantitatively describe disability and caregiving before and after LTCF entry, comparing nursing home (NH), assisted living (AL), and independent living (IL) entrants.
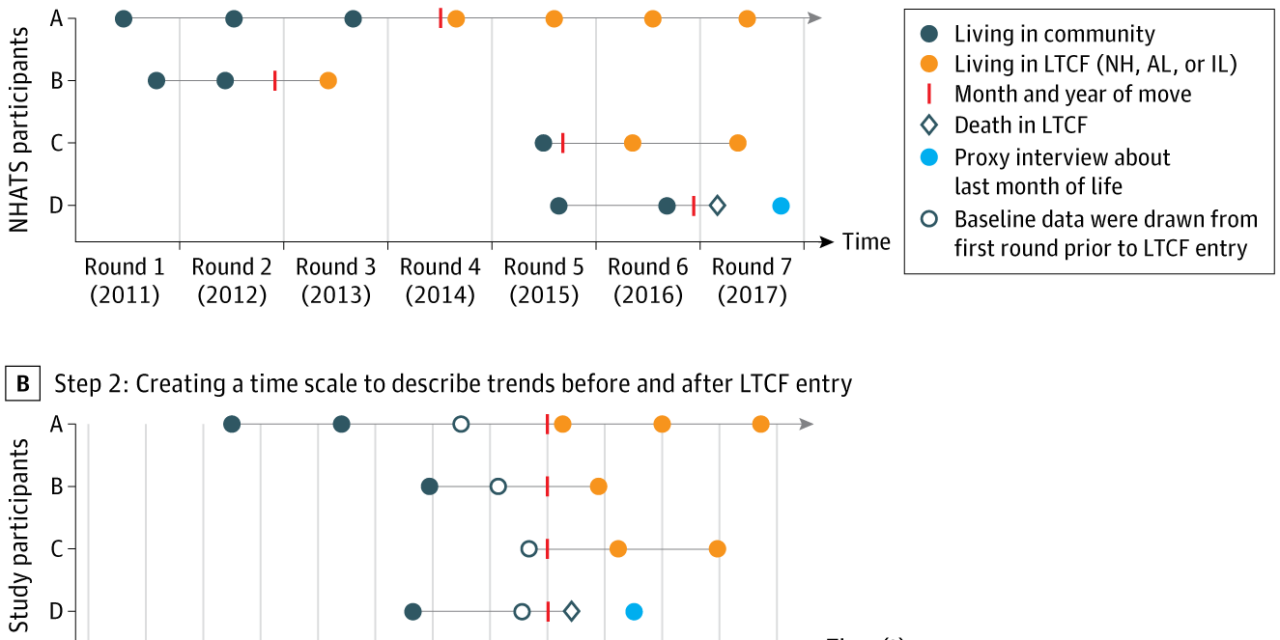
Design, Setting, and Participants
A longitudinal cohort study using prospectively collected annual data from the National Health and Aging Trends Study from 2011 to 2020 including participants in the continental US. Overall, 932 community-dwelling Medicare beneficiaries entering LTCF from 2011 to 2019 were included. Entry into LTCF was set as t = 0, and participant interviews from 4 years before and 2 years after were used.
Main Outcomes and Measures
Prevalence of severe disability (severe difficulty or dependence in ≥3 activities of daily living), prevalence of caregivers, and median weekly caregiving hours per entrant, using weighted mixed-effects regression against time as linear spline.
Results
At entry, mean (SD) age was 84 (8.4) years, 609 (64%, all percentages survey weighted) were women, 143 (6%) were Black, 29 (3%) were Hispanic, 30 (4%) were other (other race and ethnicity included American Indian, Asian, Native Hawaiian, and other), and 497 (49%) had dementia. 349 (34%) entered NH, 426 (45%) entered AL, and 157 (21%) entered IL. Overall, NH and AL entry were preceded by months of severe disability and escalating caregiving. Before entry, 49% (95% CI, 29%-68%) of NH entrants and 10% (95% CI, 3%-24%) of AL entrants had severe disability. Most (>97%) had at least a caregiver, but only one-third (NH, 33%; 95% CI, 20%-50%; AL, 33%; 95% CI, 24%-44%) had a paid caregiver. Median care was 27 hours weekly (95% CI, 18-40) in NH entrants and 18 (95% CI, 14-24) in AL entrants. On NH and AL entry, severe disability rose to 89% (95% CI, 82%-94%) and 28% (95% CI, 16%-44%) on NH and AL entry and was 66% (95% CI, 55%-75%) 2 years after entry in AL residents. Few IL entrants (<2%>
Conclusions
This study found that persons often enter NHs and ALs after months of severe disability and substantial help at home, usually from unpaid caregivers. Assisted living residents move when less disabled, but approach levels of disability similar to NH entrants within 2 years. Data may help clinicians understand when home supports approach a breaking point.