Laws in many states require notifying women if they have dense breasts, a risk factor for breast cancer. But density shouldn’t be the only factor in determining whether supplemental screening is warranted, reported researchers in a large new study led by UC San Francisco and UC Davis.
Body mass index (BMI) should also be considered, the researchers say. Their study analyzed more than 2.6 million breast density measurements at 140 radiology facilities around the country.
The study published Wednesday, June 7, 2023 in Cancer, Epidemiology, Biomarkers & Prevention, a journal of the American Association for Cancer Research.
“The goal of breast notification laws is to identify women who are at increased risk of breast cancer and might benefit from supplemental imaging,” said lead author Karla Kerlikowske, MD, a UCSF professor in the Departments of Medicine and Epidemiology and Biostatistics.
“But we found that incorporating breast density and BMI would better identify women with high breast density at risk of a missed or advanced cancer rather than using breast density alone,” she said.
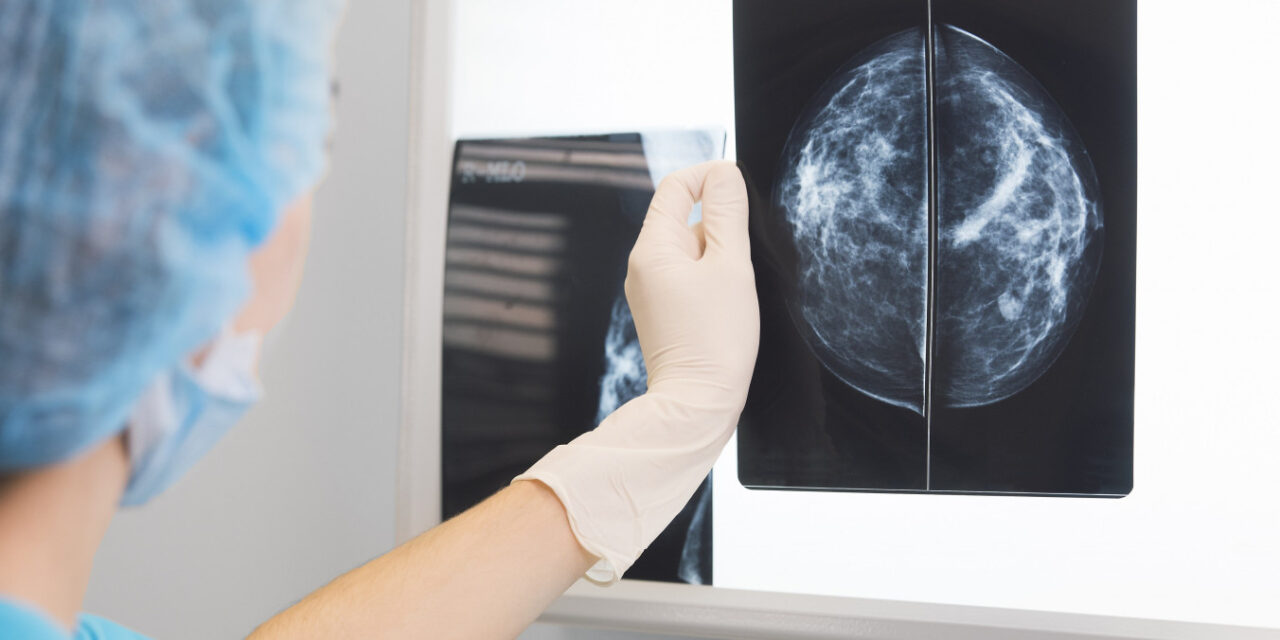
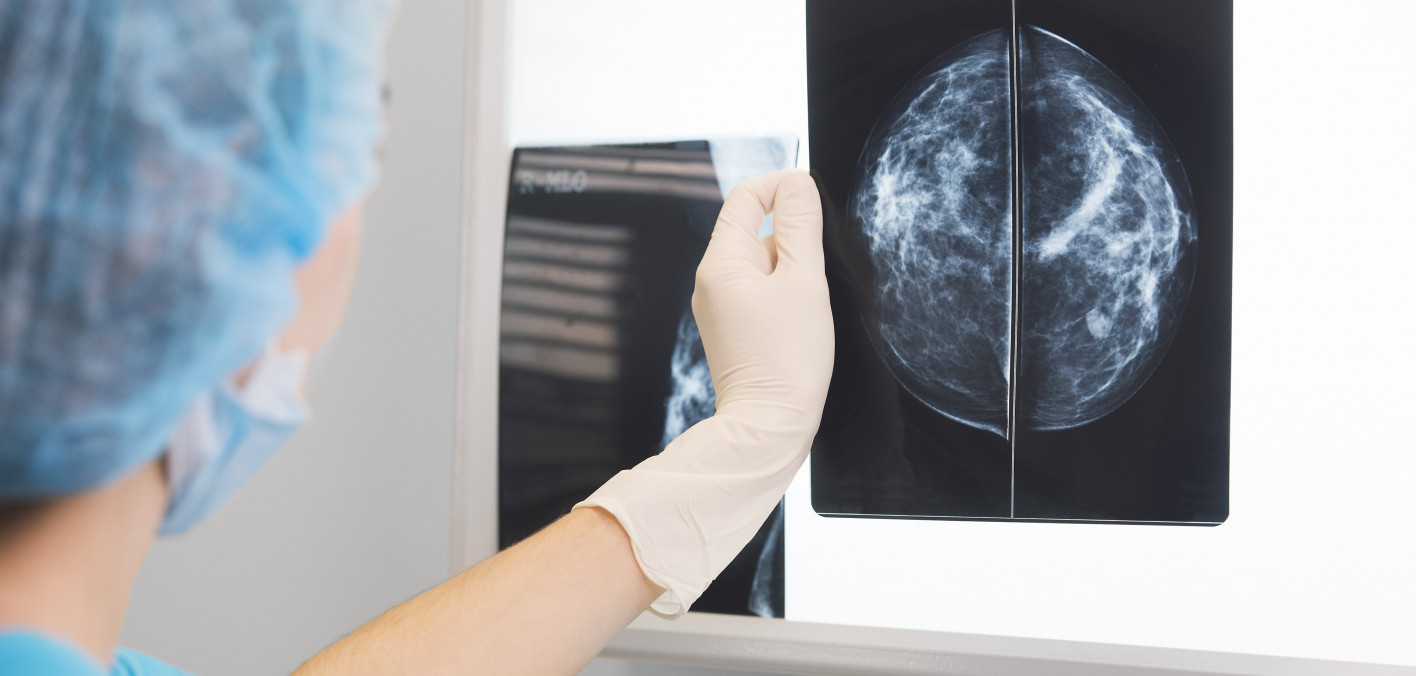
Dense breasts – those containing a high proportion of glands and connective tissue compared to fatty tissue – are common, occurring in an estimated 50% of women in their 40s, 40% in their 50s, and 25% of women older than 60. Density can make it more difficult to detect breast cancer and increases breast cancer risk, both of which suggest that additional imaging can improve early diagnosis of the disease.
At least 38 states in the U.S. have enacted laws requiring women to be notified if they have dense breasts. Additionally, the FDA announced in March new regulations taking effect September 10, 2024, that will require patients to be informed about their breast density, and to spell out that dense breasts can mask tumors and increase breast cancer risk.
Equitable screening across racial and ethnic groups
Prior small studies have shown that breast density varies across racial and ethnic groups. But these studies did not take into account multiple racial and ethnic groups or BMI.
The researchers analyzed density measurements of some 866,000 women in the Breast Cancer Surveillance Consortium from January 2005 through April 2021. The women were 40 to 74 years old and had no personal history of breast cancer.
The data showed significant differences in breast density among different racial/ethnic groups. Asian women had the largest prevalence of dense breasts, followed by white women, Hispanic/Latina women, and Black women. Obesity was most prevalent in Black women, followed by Hispanic/Latina women, white and Asian women.
These differences in breast density prevalence were clinically important and were attenuated after adjusting for age, menopausal status and BMI. The researchers said this adds to the urgency to use both BMI and breast density when deciding whom to notify about dense breasts.
“Asian women may be notified and receive a recommendation for supplemental imaging too often, while Black women with higher BMI but lower density may not be notified or receive a recommendation for supplemental imaging often enough that they are at higher risk of breast cancer and advanced breast cancer despite routine screening,” said co-lead author Michael C. S. Bissell, PhD, a biostatistician and epidemiologist at UC Davis.
Added Kerlikowske, “If breast density is the sole criterion used to notify women, it may result in implementing inequitable screening strategies across racial and ethnic groups.”
This story was published by the University of California San Francisco on June 8, 2023. It is republished with permission.