Black and Hispanic patients have a higher risk of death from second primary cancers than White and Asian/Pacific Islander patients, according to a study published in JAMA Network Open.
The study included patients diagnosed with the most common second primary cancers at 20 years of age or older from January 2000 to December 2013.
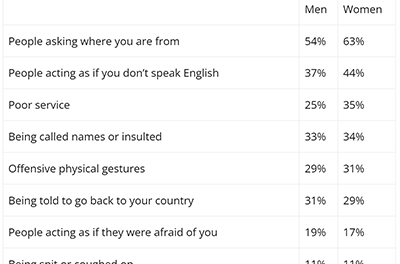
There were 230,370 patients — 79.5% of them White, 9.6% Black, 6.4% Hispanic, and 4.5% Asian or Pacific Islander. The White patients were more likely to be diagnosed with localized-stage second primary cancers (55.0%), compared to the Hispanic (51.2%), Asian/Pacific Islander (50.6%), or Black (48.1%) patients.
Continue Reading
The researchers noted that Black and Hispanic women in particular were more likely than White women to present with aggressive cancers. For example, the rate of hormone receptor-negative breast cancer was 29.6% in Black women, 22.2% in Hispanic women, and 15.9% in White women.
At a median follow-up of 54 months, 47.6% of patients had a cancer-related death, and 7.9% had a cardiovascular-related death.
The 5-year relative survival rate was highest in the White patients (60.6%), followed by the Asian/Pacific Islander patients (59.3%), Hispanic patients (58.1%), and Black patients (50.6%).
The White population had the highest survival rate for 8 of the 13 second primary cancers — female breast, oral cavity/pharyngeal, prostate, thyroid, uterine, and bladder cancer as well as melanoma and non-Hodgkin lymphoma.
The Asian/Pacific Islander population had the highest survival rate for 4 second primary cancers — colorectal, pancreatic, stomach, and lung cancer — but they had the lowest survival rate for thyroid cancer.
The Black population had the highest survival rate for kidney cancer but the lowest survival rate for 10 of the cancers — female breast, colorectal, uterine, oral cavity/pharyngeal, lung, pancreatic, stomach, bladder, and prostate cancer as well as melanoma.
Hispanic patients had the lowest survival rate for kidney cancer and non-Hodgkin lymphoma.
In an analysis adjusted for sex, age, year, and prior cancer type and stage, the risk of cancer-related death was higher in the Black population (hazard ratio [HR], 1.21; 95% CI, 1.18-1.23) and in the Hispanic population (HR, 1.10; 95% CI, 1.07-1.13) than in the White population.
The risk of cancer-related death was lower in the Asian/Pacific Islander population than in the White population (HR, 0.93; 95% CI, 0.90-0.96).
The Black population had an increased risk of cardiovascular-related death when compared to the White population (HR, 1.41; 95% CI, 1.34-1.49).
However, the risk of cardiovascular-related death was lower in the Asian/Pacific Islander population (HR, 0.75; 95% CI, 0.69-0.81) and the Hispanic population (HR, 0.90; 95% CI, 0.84-0.96) than in the White population.
“Over 20% of newly diagnosed cancers in the US occur among persons with a cancer history, and the proportion is expected to increase, highlighting a critical need to better understand outcomes in persons with multiple primary cancers,” the researchers wrote. “[T]he findings of racial and ethnic disparities in SPC [second primary cancer] survival may inform the development and equitable implementation of survivorship and treatment guidelines for the growing population of persons with multiple primary cancers.”
Reference
Sung H, Nisotel L, Sedeta E, Islami F, Jemal A. Racial and ethnic disparities in survival among people with second primary cancer in the US. JAMA Netw Open. Published online August 4, 2023. doi:10.1001/jamanetworkopen.2023.27429