Heart and blood vessel diseases already are the leading killers of Americans. They become deadlier as patients age. With so many of us growing older and into unhealthy habits, experts fear the onset of a cardiac crunch, with more and more patients struggling with heart diseases — conditions that individuals can do much to prevent.
Women are at high risk. So are blacks and Latinos, disproportionately. The perils of heart problems, researchers say, were underscored by the terrible toll inflicted by the coronavirus pandemic on older people.
The steps that older folks take to battle heart problems also can be beneficial to their overall health, including cognitive function and sense of well-being. They involve common sense and are not difficult to follow. Here are key takeaways about staying heart healthy.
Age is a big factor in heart disease
The human heart performs nothing less than a miracle: every second, every day, for our lifetimes.
With a per-beat force equal to firmly squeezing a tennis ball, the heart pumps roughly six quarts of lifegiving blood throughout the body, beating around 100,000 times in a day, 35 million times in a year, and more than 2.5 billion times during an average lifespan.
It should come as no surprise that this muscle and the pipes tied to it (our veins and arteries) cannot perform at peak levels forever. They deteriorate over time.
This is not only an individual issue but a huge medical worry as the giant baby boom generation grays fast, with an estimated 10,000 of them reaching retirement age every day from Jan. 1, 2011, to Dec. 31, 2030.
The soaring number of seniors and their potential declines in heart health alone will be “exacting an enormous toll on the health and quality of life of older Americans,” Judith Graham, a columnist of aging issues for the Kaiser Family Foundation Health News group, reported, based on interviews with experts. As she wrote:
“The estimates are sobering: By 2060, the prevalence of ischemic heart disease (a condition caused by blocked arteries and also known as coronary artery disease) is projected to rise 31% compared with 2025; heart failure will increase 33%; heart attacks will grow by 30%; and strokes will increase by 34%, according to a team of researchers from Harvard and other institutions. The greatest increase will come between 2025 and 2030, they predicted.”
Of course, forecasts can be wrong. Medical science could find breakthrough treatments for heart and vascular ills. But the experts, she noted, already have major research to cause growing worries:
“More than 80% of cardiovascular deaths occur among adults 65 or older. For about a dozen years, the total number of cardiovascular deaths in this age group has steadily ticked upward, as the ranks of older adults have expanded and previous progress in curbing fatalities from heart disease and strokes has been undermined by Americans’ expanding waistlines, poor diets, and physical inactivity. Among people 65 and older, cardiovascular deaths plunged 22% between 1999 and 2010, according to data from the National Heart, Lung, and Blood Institute — a testament to new medical and surgical therapies and treatments and a sharp decline in smoking, among other public health initiatives. Then between 2011 and 2019, deaths climbed 13%.”
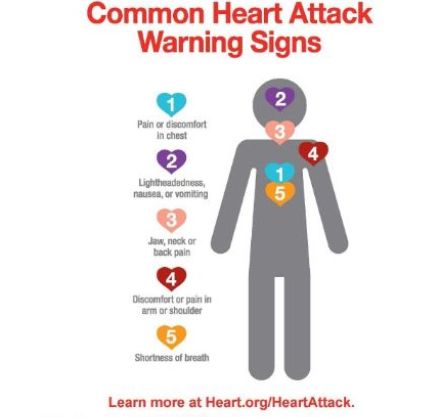
Graphic, above, courtesy, American Heart Association.
Risks higher for black and Latino patients
The pandemic laid bare the big cardiac risks confronting black and Latino patients, especially as they age.
They suffer heart disease in disproportionate numbers, worsened by their propensities — as individuals and groups — to struggle with common aggravating conditions: high blood pressure, diabetes, and excessive weight. As columnist Graham reported:
“Because the risk factors [for heart disease] are more common among black and Hispanic populations, cardiovascular illness and death will become even more common for these groups, the researchers predicted. (Hispanic people can be of any race or combination of races.) ‘Disparities in the burden of cardiovascular disease are only going to be exacerbated’ unless targeted efforts are made to strengthen health education, expand prevention, and improve access to effective therapies, wrote the authors of an accompanying editorial [to published research on the threat of soaring cardiovascular problems in older adults], from Stony Brook University in New York and Baylor University Medical Center in Texas.”
Cardiologists have warned for a while about medical and social inequities that make patients of color more vulnerable. In 2017, the American Heart Association published a scientific statement describing cardiovascular disease disparities for blacks, finding that racism and the stress related to it appear to aggravate racial minorities problems with “hypertension, obesity, persistent inflammation, and other clinical processes,” Graham noted.
The scientific statement, detailed and covering a range of issues, urges the U.S. medical establishment to take extensive steps to improve the problems that undercut the health and longevity of black patients, reporting:
“There are marked disparities in the onset of heart failure, stroke, and peripheral vascular disease between African Americans and whites … However, mortality from all [cardiovascular diseases] is significantly higher in African Americans compared with whites, which suggests a role for health care to mitigate disparities with comprehensive screening, an enhanced specificity of diagnoses, and tailored disease management.”
The pandemic added even greater urgency to the importance of U.S. medicine in dealing with racial inequities, with African American and Latino patients suffering disproportionate coronavirus infections, debilitation, and deaths, as Graham reported:
“The pandemic laid bare ongoing health inequities,” and that has fueled a new wave of research into disparities across various medical conditions and their causes, said Nakela Cook, a cardiologist and executive director of the Patient-Centered Outcomes Research Institute, an independent organization authorized by Congress.
For older women, special challenges
Older women confront special heart health challenges that increase with age.
Women lose protective benefits of hormones after menopause, and they live longer than men do — factors increasing their cardiovascular challenges. As one published study from Florida researchers reported:
“While age is an independent risk factor for [heart and circulatory diseases], other additional risk factors that are closely associated with advanced age have been shown to compound these risks, including frailty, obesity, and diabetes … females have a longer life expectancy than males [and] women make up the most significant percentage of [cardiovascular disease] diagnoses in the elderly population, or in those greater than 80 years old … Gender is yet another major risk factor regarding the onset, manifestation, and management of [cardiovascular disease] in aging adults. The decline in hormone levels may play a significant role in [its] development … but hormone replacement therapies have not yet shown a significant benefit in older adults, with respect to cardiovascular health.”
Women must deal with major gaps in their awareness about and medical treatment for heart and circulatory issues, experts say. As the New York Times reported:
“[S]tudies have long shown that women are more likely than men to dismiss the warning signs of a heart attack, sometimes waiting hours or longer to call 911 or go to a hospital. Now researchers are trying to figure out why. They have found that women often hesitate to get help because they tend to have more subtle heart attack symptoms than men — but even when they do go to the hospital, health care providers are more likely to downplay their symptoms or delay treating them. Health authorities say that heart disease in women remains widely underdiagnosed and undertreated and that these factors contribute to worse outcomes among women and heightened rates of death from the disease.
“Most studies suggest that a major reason women delay seeking care — and are often misdiagnosed — is because of the symptoms they develop. While chest pain or discomfort is the most common sign of a heart attack in both sexes, women who have heart attacks are far less likely than men to have any chest pain at all. Instead, they often have symptoms that can be harder to associate with cardiac trouble, like shortness of breath, cold sweats, malaise, fatigue, and jaw and back pain.
“A report by the American Heart Association found that heart attacks are deadlier in women who do not exhibit chest pain, in part because it means both patients and doctors take longer to identify the problem. But when women suspect they are having a heart attack, they still have a harder time getting treated than men do. Studies show they are more likely to be told that their symptoms are not cardiovascular related. Many women are told by doctors that their symptoms are all in their head. One study found that women complaining of symptoms consistent with heart disease — including chest pain — were twice as likely to be diagnosed with a mental illness compared to men who complained of identical symptoms.”
Patients — men and women — should try to be as detailed and specific as possible about their problems and concerns when seeing their doctors, including what they’re doing when symptoms show up.
Doctors and nurses who are dismissive about the possibility of heart disease should get their own dismissal: from treating you. Patients should not tolerate medical “gaslighting,” which seems to be the current way of describing bad medicine and practices that could lead negligent caregivers into needless mistreatment of their patients with preventable tragedies.
Common sense in prevention and care
While doctors, researchers, and policy makers express increasing fears about older Americans’ cardiovascular disease challenges, don’t forget that these problems start early.
They can be reduced and maybe even averted.

The American Heart Association has issued what it calls its “essential eight” ways to pursue longer, healthier lives without the burdens of cardiovascular diseases and conditions. In brief, the heart experts recommend that all of us:
Watch your weight. Don’t smoke or vape. Eat in moderation, consuming more plants, nuts, and sustainable fish. Avoid red meat, excess sugar and salt, and highly processed junk food. Get lots of restful sleep.
The heart association’s recently suggested goal, the Washington Post reported, “is seven to nine hours of sleep daily for adults, and more for children (eight to 10 hours for 13- to 18-year-olds, nine to 12 hours for 6- to 12-year-olds and 10 to 16 hours for children 5 and younger).”
More on the Life’s Essentials list:
We all need vigorous and regular exercise. Cut down on the booze and other intoxicants, as well as the stress. Be social and don’t let yourself get lonely, isolated, and depressed.
Work with your primary care doctor or cardiologist to control your blood pressure, blood sugar, and cholesterol. Patients may be prescribed medications that can bolster their efforts to deal with these harmful conditions. They need to ask questions about any drugs ordered for them — and they need to be sure to take their meds to see benefits.
Research shows that 62% of patients with serious, chronic conditions said in a survey that they didn’t take prescribed medications because they just forgot to do so. Caregivers discovered, to their distress, that 28% of those studied had run out of meds and had not told their MDs they needed refills. As the American Heart Association said in a recent policy statement:
“Medications do not work in patients who do not take them. Non-adherence is one of the largest challenges faced by [medical] providers in their management of [patients’] chronic illness.”
By the way, sticking to healthful habits can benefit not only your heart but your overall wellness and longevity. As the New York Times reported:
“[T]he big enchilada [for a long, healthy life], as [an] extraordinarily comprehensive study clearly demonstrate[d], is how people live their lives: whether they smoke, what and how much they eat, and whether they abuse alcohol or drugs. These, along with high levels of blood sugar and blood pressure, both of which are influenced by diet, are the main factors dictating poor health. ‘About three-fourths of the variation in life expectancy between counties can be explained by these big risk factors,’ Dr. [Christopher J.L.] Murray, epidemiologist and health economist at the University of Washington, said in an interview … Alas, the study [in which Murray was lead author] did not measure the contribution of regular exercise to longevity and long-lasting health. “There’s not as much research on the effects of physical activity as there should be,” Dr. Murray said …”
Graphic, above, courtesy American Heart Association
A change in approach could boost supply of hearts for transplant
While tens of thousands of patients across the country with grievous heart problems wait and hope for organs, just over 4,000 transplants were performed in 2022.
That was a record number.
Still, a shortage of suitable donor hearts leaves too many people in need, though researchers say they have hope for a different approach to surgical considerations that could increase the national supply by as much as 30%.
Investigators have shown that hearts once thought to be unusable can be “reanimated” in a short period after a donor is declared dead, typically due to nonsurvivable brain injury. As the Associated Press reported:
“The usual method of organ donation occurs when doctors, through careful testing, determine someone has no brain function after a catastrophic injury — meaning they’re brain-dead. The body is left on a ventilator that keeps the heart beating and organs oxygenated until they’re recovered and put on ice. In contrast, donation after circulatory death occurs when someone has a nonsurvivable brain injury but, because all brain function hasn’t yet ceased, the family decides to withdraw life support and the heart stops. That means organs go without oxygen for a while before they can be recovered — and surgeons, worried the heart would be damaged, left it behind. What’s changed: Now doctors can remove those hearts and put them in a machine that ‘reanimates’ them, pumping through blood and nutrients as they’re transported –- and demonstrating if they work OK before the planned transplant.”
In a nationwide trial, in multiple sites, surgeons tested the transplanting of hearts using the different approach, finding six-month outcomes compared favorably to previous techniques: 94% survival for recipients of cardiac-death donations and 90% for those who got the usual hearts, according to a study published in the New England Journal of Medicine.
Research experts cautioned that more study is needed, especially because the latest surgical trial was not randomized and blinded. Surgeons also did not transplant hearts harvested in the new way into patients in the weakest and riskiest status. They did find that 90% of hearts recovered in a new way proved suitable for transplantation.
As the AP noted:
“The findings are exciting and show ‘the potential to increase fairness and equity in heart transplantation, allowing more persons with heart failure to have access to this lifesaving therapy,’ transplant cardiologist Dr. Nancy Sweitzer of Washington University in St. Louis, who wasn’t involved with the study, wrote in an accompanying editorial.”
Recent Health Care Developments of Interest
Here are some recent news articles on health and medical topics that might interest you:
§ The all-too-familiar body mass index aka the BMI? Forget about it as the sole and leading measure of patients’ weight and wellness, the American Medical Association has declared. The influential doctors’ group says the BMI, a calculation of weight in kilograms divided by height in meters, is inaccurate and racially discriminatory. The metric, the New York Times reported, has become a guide star for too many lay folks and practitioners in deciding whether and when to undertake weight loss programs. The AMA, instead, says doctors should “consider factors like someone’s visceral fat (the fat stored in the abdominal cavity and around the organs), body adiposity index (a calculation that uses hip circumference and height), the percentage of fat, bone and muscle in one’s body and genetic and metabolic factors, like abnormal blood sugars or thyroid tests.”
§ Despite the years of a huge public policy focus on improving its access and affordability, U.S. health insurance persists as a problem for patients seeking medical care. As the New York Times reported: “A majority of Americans with health insurance said they had encountered obstacles to coverage, including denied medical care, higher bills, and a dearth of doctors in their plans, according to a new survey from KFF, a nonprofit health research group. As a result, some people delayed or skipped treatment. Those who were most likely to need medical care — people who described themselves as in fair or poor health — reported more trouble; three-fourths of those receiving mental health treatment experienced problems.
§ Players, especially in the age 60-plus group, may be getting themselves into a medical pickle with increasingly common injuries due to pickleball. The court and paddle game — a fad among millions of affluent and older folks — “will lead to: 67,000 emergency department trips, 366,000 outpatient visits, 8,8000 outpatient surgeries, 4,700 hospitalizations and 20,000 post-acute episodes,” according to UBS analysts, quoted by Forbes. The experts at the bank and financial firm estimate that “Americans will spend between $250 million and $500 million in costs tied to pickle injuries this year.”
§ It just makes you say, “Hmmm….” As part of its deep digging into a giant trove of Internal Revenue Service records on the taxes of the wealthiest among us, the Pulitzer Prize-winning investigative site ProPublica finds that the bigs who run relatively small biotech and healthcare enterprises like medical device makers and drug companies are leaders among all industry titans in having remarkable good fortune with sector stocks. “Dozens of wealthy executives and well-connected investors reported superbly timed stock trades in such companies, including in businesses they competed with or had personal ties to,” ProPublica reported.
§ With billions of dollars committed to battling the opioid drug crisis — which has claimed almost 1 million lives since 1999 and continues to kill just under 100,000 Americans annually — just how are states and local governments spending $50 billion in settlements struck with various parties in Big Pharma to help remedy damages? The nonprofit, independent KFF Health News organization and a web-based operation called OpioidSettlementTracker.com have pledged to act as watchdogs over big sums described already as double NASA’s budget and five times the revenue of an NBA season. This initiative bears watching, especially as excellent reporting by the Associated Press is showing taxpayers how billions of dollars in coronavirus pandemic aid got ripped off by a veritable army of grifters.
HERE’S TO A HEALTHY (REST OF) 2023!
Sincerely,

Patrick Malone
Patrick Malone & Associates