August 08, 2023
6 min read
A 38-year-old woman was referred to the retina service at the Lahey Hospital & Medical Center’s department of ophthalmology by a retina specialist for temporal flashes and a stationary black spot in the left eye for 1.5 months.
She denied blurred or double vision, floaters, eye redness, pain with eye movements, or change in color vision. Review of systems was negative for recent travel, tick bites, skin rashes and cough and positive for joint pain in her fingers.
Source: Julia Watson, MD, and Kendra Mascia-Klein, MD
Her medical history included Bell’s palsy 8 years prior and gluten intolerance. Her family history was significant for a variety of autoimmune diseases in maternal aunts and cousins, including systemic lupus erythematosus, scleroderma and Hashimoto’s thyroiditis. She did not take any regular medications and had no known drug allergies. She denied smoking, drug or alcohol use.


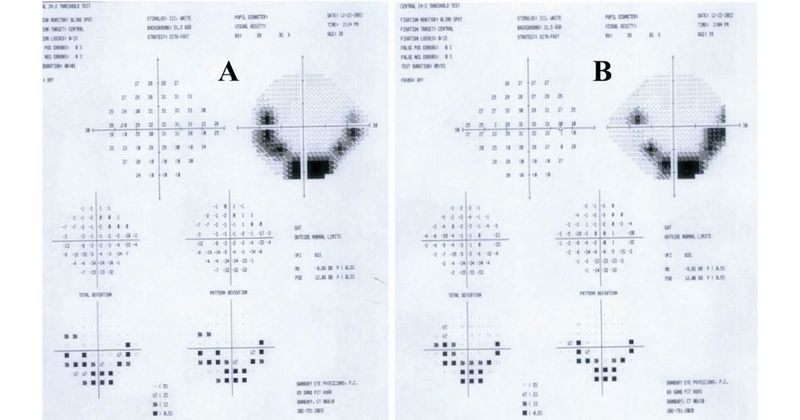
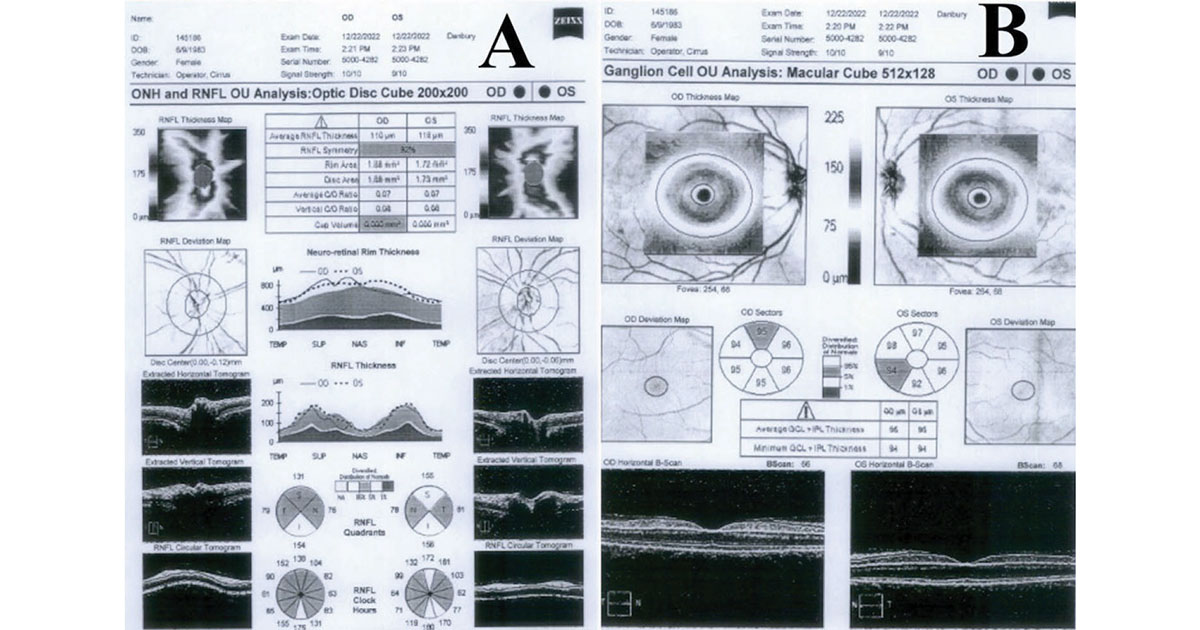
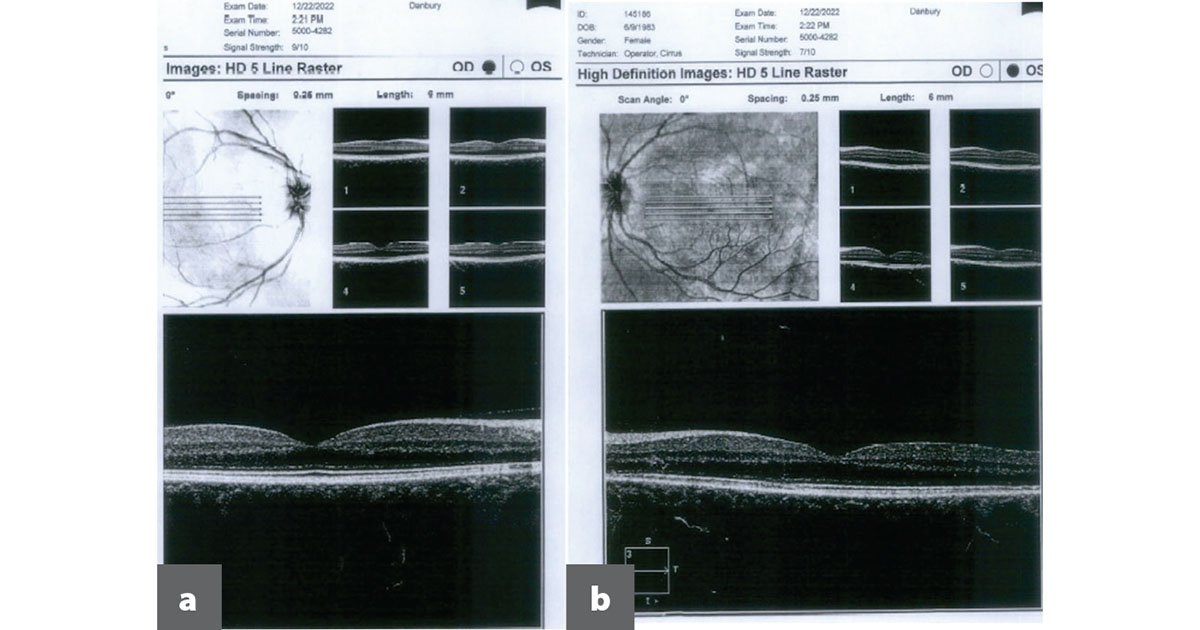
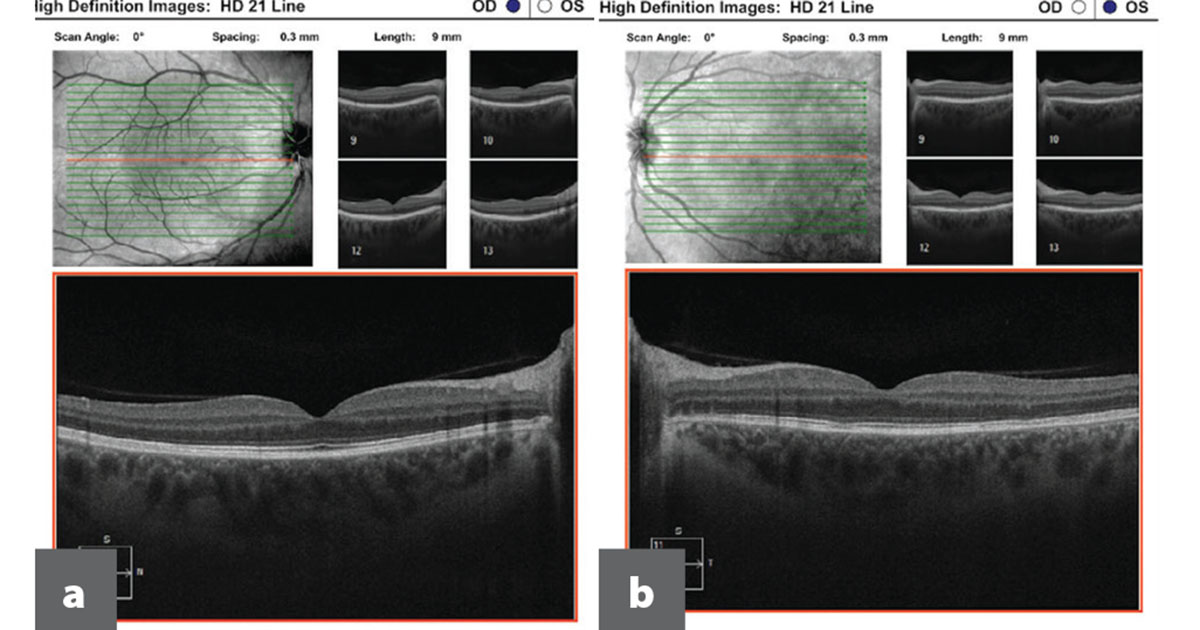
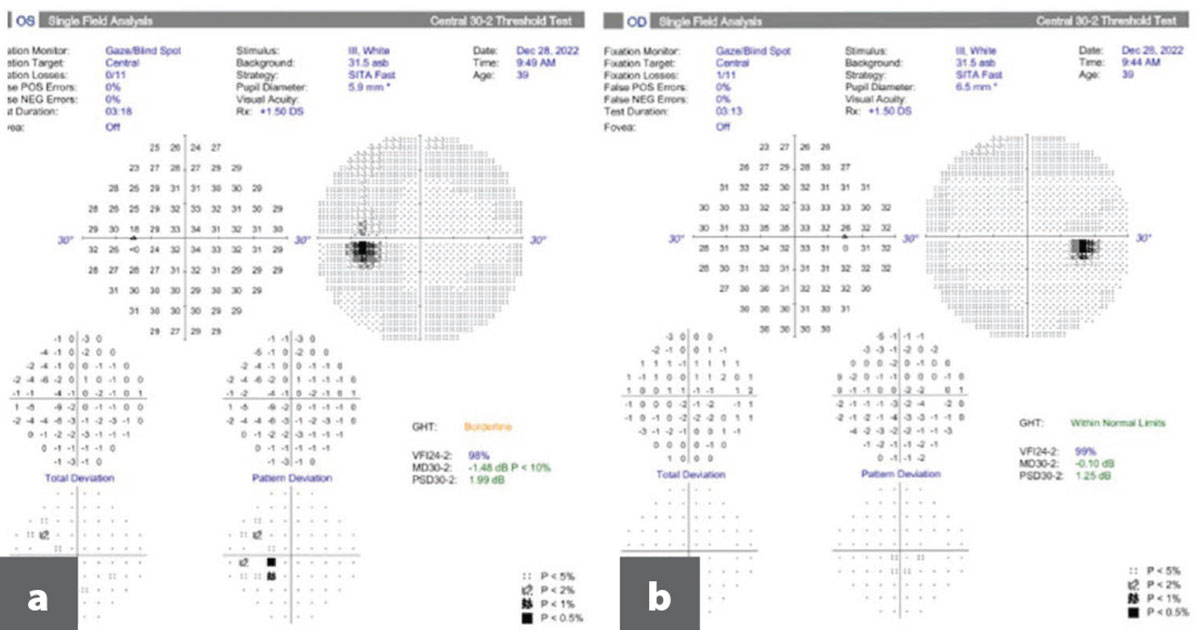
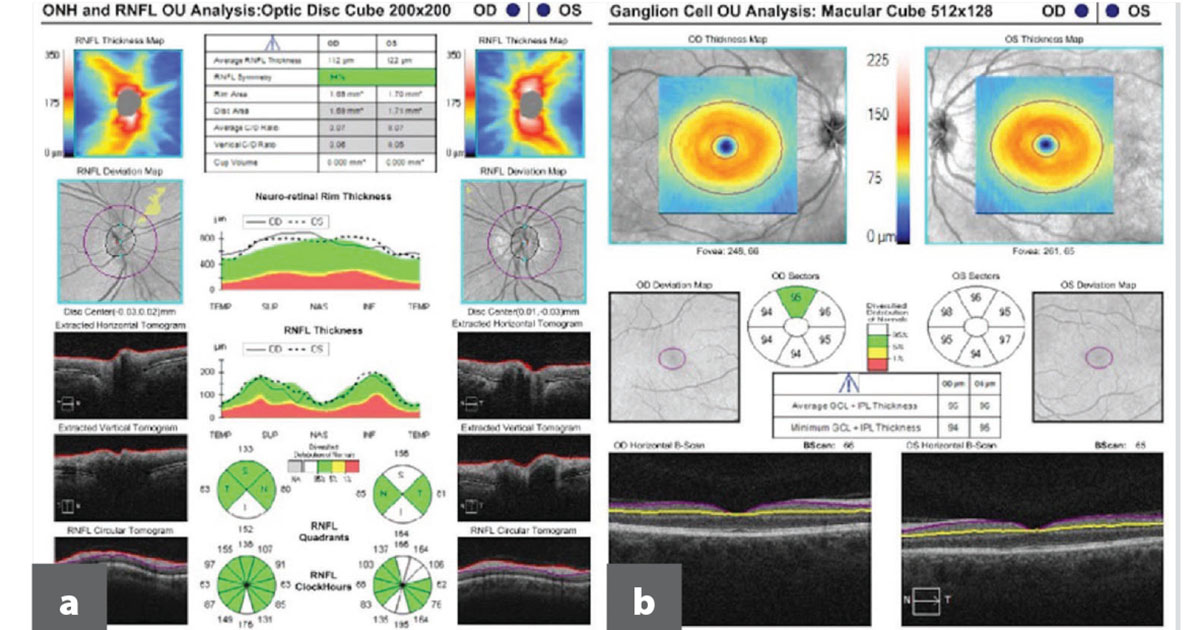
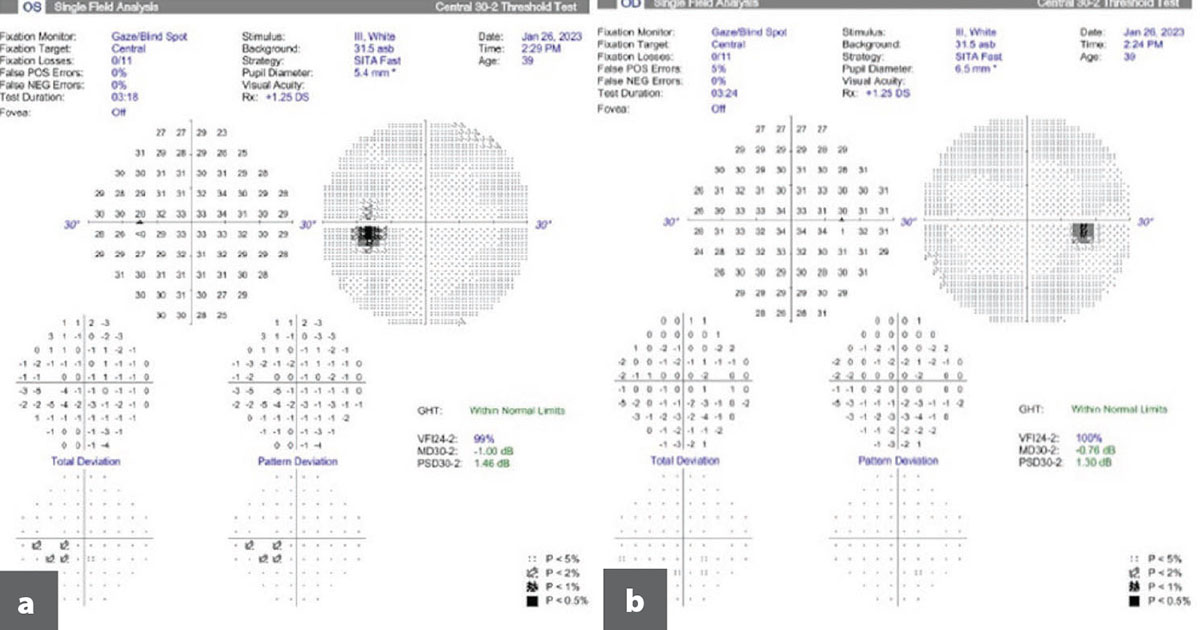
She was not on any ophthalmic medications and had no prior ophthalmic surgeries. An outside retinal provider saw her twice in the month before her presentation at Lahey. In the first evaluation for photopsias and scotoma in the left eye, dilated fundus exam was negative for retinal tear or detachment. In the second evaluation for persistent symptoms, her symptoms were suspected to be secondary to vitreous traction vs. atypical migraine. Outside testing was reviewed before evaluation at Lahey. Humphrey Visual Field (HVF) 30-2 showed fairly symmetric bilateral inferior defects resembling inferior arcuate scotomas (Figures 1a and 1b). OCT retinal nerve fiber layer (RNFL) and ganglion cell analysis were unremarkable (Figures 2a and 2b). OCT macula showed possible inner segment/outer segment (IS/OS) disruption parafoveally nasally in the left eye (Figure 3b).
Examination
On exam at Lahey Hospital, the patient’s best corrected visual acuity was 20/25 in the right eye and 20/30+ in the left eye. Pupils were equally round and reactive to light without afferent pupillary defect. IOP measured by iCare tonometer was 13 mm Hg in the right eye and 15 mm Hg in the left eye. Color vision was full by Ishihara color plates. Confrontation visual fields were full in both eyes. Extraocular movements were full with orthotropic alignment.
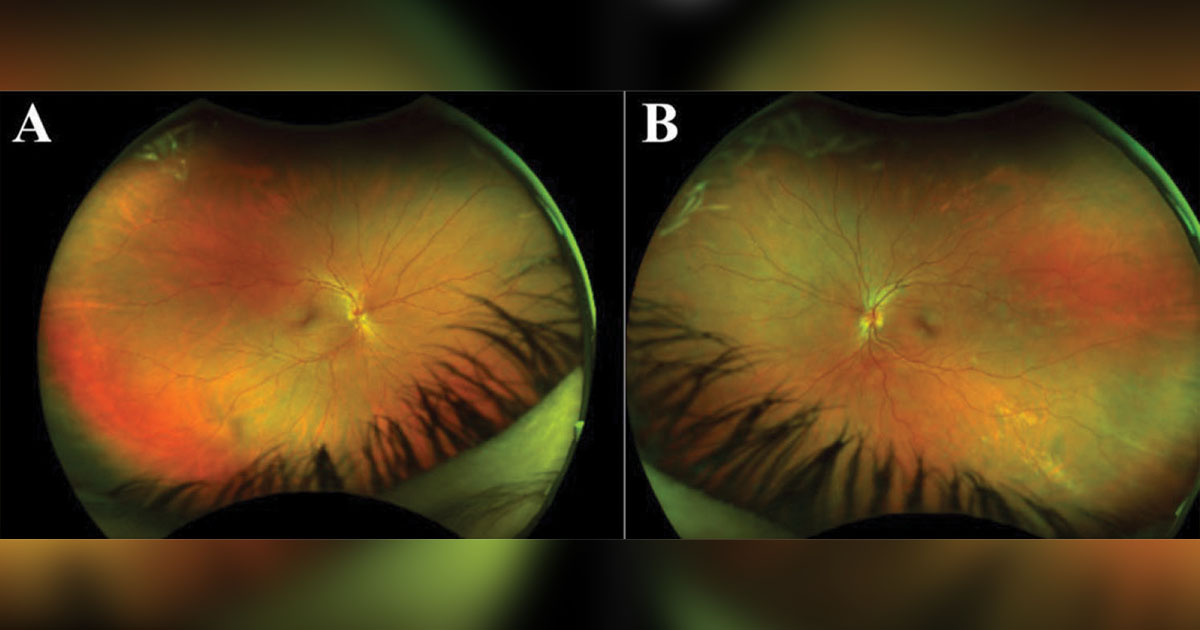
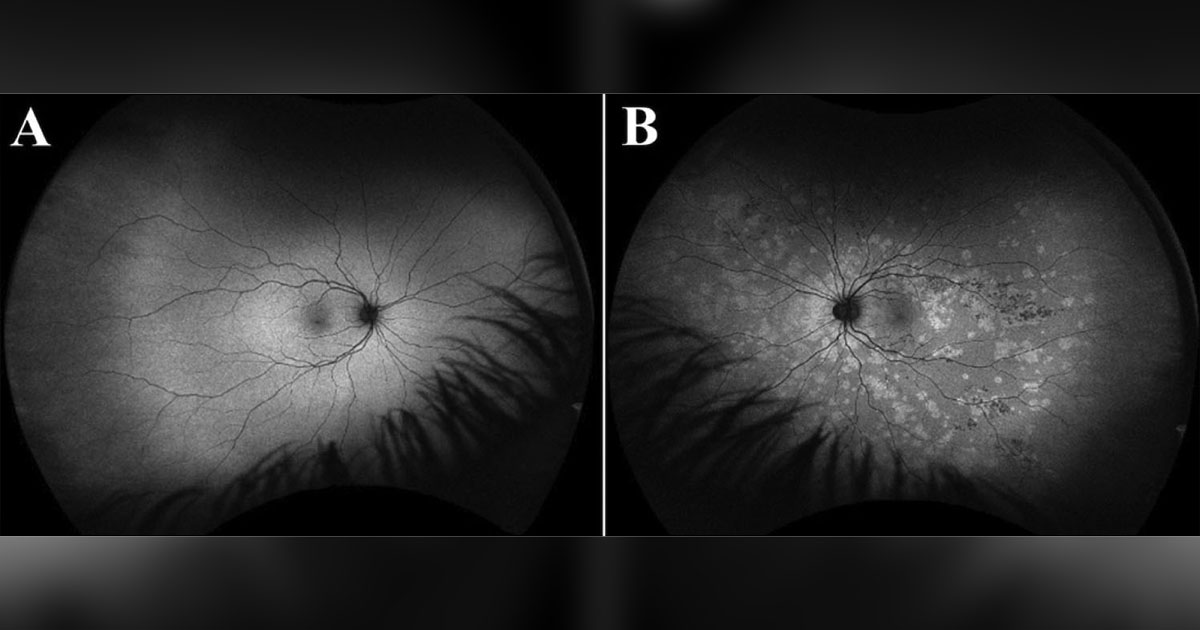
Anterior segment slit lamp exam was unremarkable in both eyes, including deep and quiet anterior chambers and clear vitreous without cells or haze. On dilated fundus exam, the optic nerves appeared pink and sharp with 0.1 cup-to-disc ratio in both eyes. The macula and periphery in the right eye were normal. The left eye showed multifocal hypopigmented spots in the macula, peripapillary and mid-periphery with scattered hyperpigmented spots/chorioretinal atrophy and retinal pigment epithelium (RPE) clumping (Figures 4a and 4b). The vessels were normal in both eyes.
Imaging
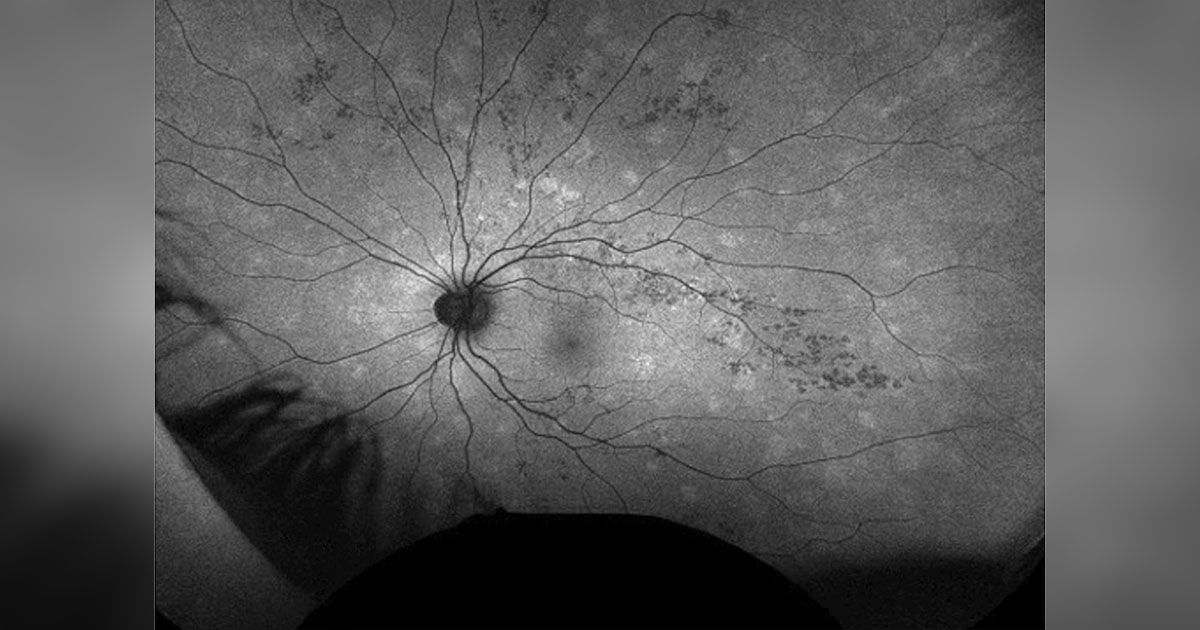
OCT macula in the right eye showed normal foveal contour without fluid or photoreceptor disruption and possible choroidal thickening, while the left eye showed discrete IS/OS disruption parafoveally and a thickened choroid (Figures 5a and 5b). HVF 30-2 was normal in the right eye (Figure 6a), while the left eye showed an enlarged blind spot (Figure 6b). OCT RNFL (Figure 7a) and ganglion cell layer analysis (Figure 7b) were unremarkable in both eyes. Fundus autofluorescence (FAF) was unremarkable in the right eye (Figure 8a), while the left eye (Figure 8b) showed numerous hyperautofluorescent spots in the peripapillary region, macula and mid-peripheral retina.
What is your diagnosis?
See answer below.
Photopsias, scotoma
In a young woman presenting with acute, painless unilateral photopsias and scotoma, multiple evanescent white dot syndrome (MEWDS) should be considered, even in the absence of characteristic fundus findings, as patients may present after the hypopigmented lesions have resolved. The differential diagnosis includes other white dot syndromes such as multifocal choroiditis (MFC), punctate inner choroidopathy (PIC), acute zonal occult outer retinopathy (AZOOR) as well as masqueraders including syphilis, sarcoidosis, Lyme and lymphoma.
Unlike MEWDS, MFC, which presents with yellowish-gray lesions at the level of the RPE and choriocapillaris, tends to occur bilaterally and is more often associated with anterior chamber and vitreous cell. PIC, typically presenting with yellow lesions smaller than 300 µm in size at the posterior pole, also tends to occur bilaterally but is less likely to have anterior or vitreous cells. Although MFC is characterized by chronic, recurrent disease and PIC is less likely to recur, both can lead to development of choroidal neovascularization with central vision loss. AZOOR, which may also present with photopsias and visual field loss, may present with a normal fundus appearance initially or with an annular whitish or gray line demarcating the border of the retinopathy. In later stages, the fundus may show zonal areas of RPE and chorioretinal atrophy and pigmentary changes, often in the peripapillary region. There can be characteristic “trizonal” features on OCT and FAF testing, which help differentiate this disease.
The masqueraders, by definition, can have similar fundus and outer retinal changes but, unlike the aforementioned entities, are more likely to present bilaterally, have significant anterior or vitreous cells, and affect older individuals who have a history of immunosuppression or malignancy. Unlike MEWDS, these entities do not spontaneously resolve without appropriate treatment.
Workup, management and follow-up
Based on our patient’s characteristic symptoms and fundus findings, a working diagnosis of MEWDS was made, and the recommendation was to observe. Although not typically necessary, a limited workup for syphilis, tuberculosis and sarcoidosis was done.
Given that the patient never had symptoms in the right eye, that her OCT RNFL and ganglion cell analyses were normal, and because the initial visual field deficits were not reproducible at our office, it was suspected the field deficits were likely an error.
The patient returned for 1-month follow-up. She reported unchanged shimmering photopsias and scotoma. On exam, uncorrected visual acuity was stable at 20/30-1 in the right eye and 20/30 in the left eye. Pupil exam was normal. IOP via iCare was stable at 16 mm Hg in the right eye and 10 mm Hg in the left eye. Confrontation visual fields and extraocular movements remained full in both eyes.
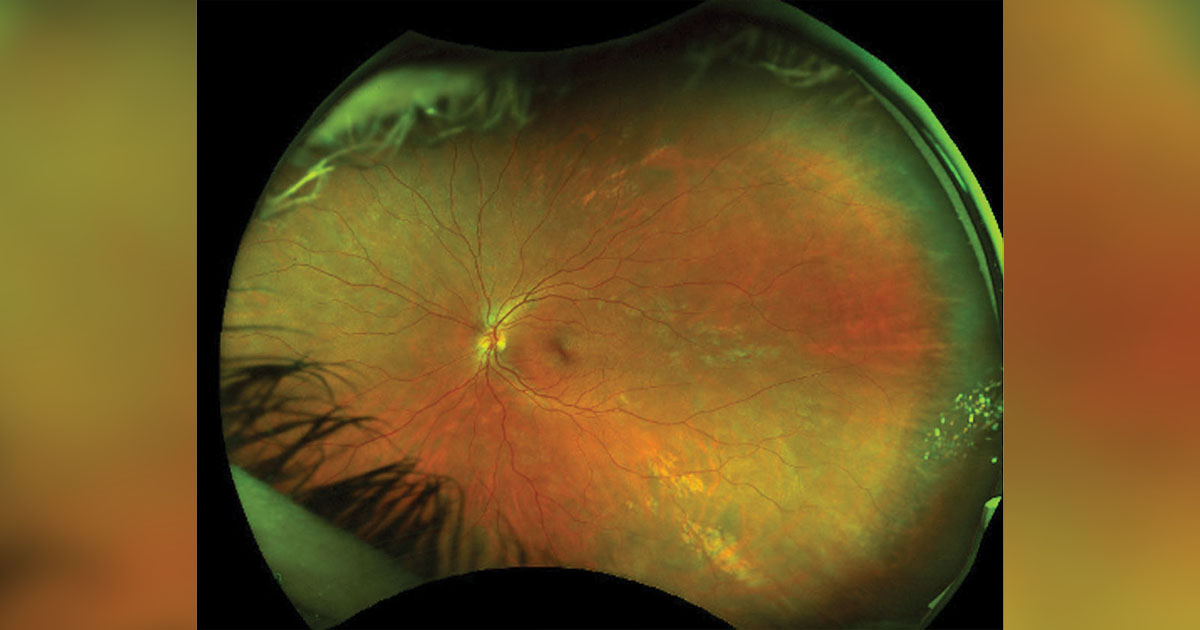
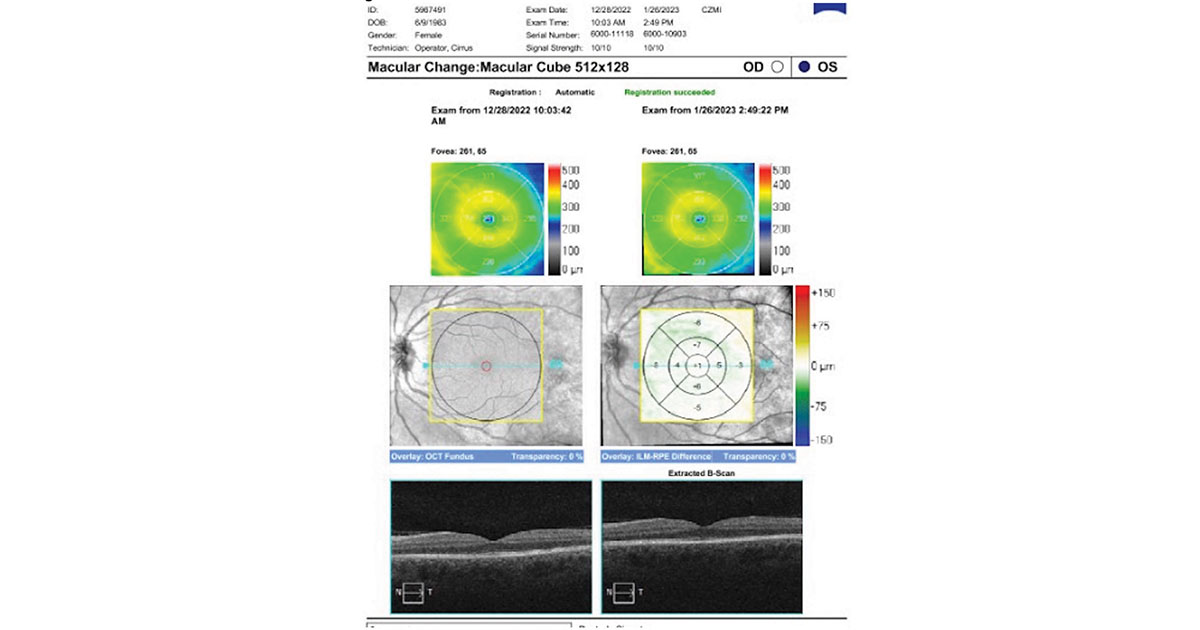
Anterior segment slit lamp exam was stable and unremarkable in both eyes. Dilated fundus exam showed improved appearance of the multifocal white dots in the left eye (Figure 9). OCT macula in the right eye was unchanged, and the left eye showed near reconstitution of the IS/OS junction (Figure 10). HVF 30-2 was again normal in the right eye (Figure 11a), and the left eye showed a persistent enlarged blind spot (Figure 11b). FAF remained unremarkable in the right eye, and the left eye showed interval improvement in the multiple hyperfluorescent spots (Figure 12).
The patient canceled her subsequent follow-up appointment but reported slight improvement in shimmering lights and scotoma.
Discussion
MEWDS commonly presents in healthy women in their 20s to 40s. Patients typically report unilateral symptoms of shimmering photopsias and a scotoma. Fifty percent of cases are preceded by a flu-like illness. On exam, the fovea often has a granular appearance that may not return to normal appearance. Visual field testing may show enlargement of the blind spot. Findings on fluorescein angiography are characterized by leakage from disc capillaries and “wreath”-like hyperfluorescence. OCT macula shows ellipsoid zone disruption. FAF shows hyperautofluorescent spots more than are seen clinically. Typically, MEWDS is self-limiting, although 10% of cases may recur. The diagnosis can be challenging due to the transient clinical findings; within 2 to 6 weeks of symptom onset, the white dots may fade. However, the temporal scotoma and photopsias can take several months to improve. Prognosis is generally good.
- References:
- BCSC. Retina and vitreous. Section 12. 2021-2022.
- Gargouri MA, et al. Ocul Immunol Inflamm. 2022;doi:10.1080/09273948.2022.2127782.
- Multiple evanescent white dot syndrome (MEWDS). https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/MEWDS/index.htm. Accessed June 28, 2023.
- Russell JF, et al. Int Ophthalmol. 2020;doi:10.1007/s10792-019-01223-4.
- Toussaint B, et al. Multiple evanescent white dot syndrome. https://eyewiki.aao.org/Multiple_Evanescent_White_Dot_Syndrome. Updated June 17, 2023. Accessed June 28, 2023.
- Yanoff M, et al. Ophthalmology. 3rd ed. Elsevier; 2009.
- For more information:
- Edited by Yi Ling Dai, MD, and Teresa P. Horan, MD, of New England Eye Center, Tufts University School of Medicine. They can be reached at ydai@tuftsmedicalcenter.org and thoran@tuftsmedicalcenter.org.




