n  n
n
n
n Part 2 of a two-part series on making decisions about driving as we age. Read Part 1 here. n
n
It’s a simple but unfortunate fact: driving skills can wane over time.
n
Eventually, driving can become unsafe for an older driver, their passengers, and others on the road. If you notice a decline in driving abilities in a loved one, or in yourself, what’s the best way to handle this?
n
If you’re an older driver: Create an action plan
n
If you’re an older driver, don’t wait for a near-miss or an accident to think about the next steps. Planning ahead can help you tackle fixable issues, make necessary transitions easier, and avoid harming yourself or someone else.
n
Here are six measures you can take right now:
n
Have a frank conversation with a trusted friend or family member. After driving with them as a passenger, ask whether they are worried about your driving. Don’t disregard their comments, even if they share things you don’t want to hear.
n
See your doctor and talk about your driving. Is it harder to see at night? Are you finding you’re slower to react? Ask your doctor about medical care that can help, such as cataract surgery, treatment for sleep apnea, or adjustments to medications that might affect driving.
n
Take a self-evaluation test or an on-road test.AAA has tools to help with this, or you can check with your local department of motor vehicles for options. Even if you feel it’s unnecessary, a driving test can be reassuring to your loved ones that you’re still safe behind the wheel.
n
Take driving classes. In many places, there are general refresher courses, courses for defensive driving, and even simulators that don’t require actual road tests. AAA and AARP offer online courses that can help you improve your driving. (And by the way, these courses may also reduce the cost of your auto insurance!)
n
Consider alternatives to how you drive. Stick to roads that are close to home or to routes that have traffic lights (rather than having to decide when traffic is clear enough to turn). Consider giving up night driving if that is particularly difficult.
n
Make adjustments to your car that can help. Examples include using a steering wheel cover to improve your grip or changing the position of your seat to improve your view of the road. Check out the CarFit program that aims to optimize the “fit” of a driver in their car.
n
In addition, explore options that don’t require you to drive as often or at all:
n
- n
- grocery delivery
- public or senior transportation (if offered or available where you live)
- carpooling with friends or family
- ride-hailing services or taxis
- hiring a driver.
n
n
n
n
n
n
Cost and availability may be barriers, but it’s worth looking into these options.
n
If you’re a concerned family member or friend: Start a conversation
n
With so much at stake, the language you use matters. So, it’s a good idea to think ahead about how to talk about these challenges.
n
Put safety and solutions first. It’s best not to lead by criticizing driving skills. Instead, talk about driving with safety and solutions in mind, such as the options described above.
n
Choose your words carefully. It helps to avoid threats or confrontational language: rather than saying “Your driving is terrible so I’ve taken away your keys,” focus on safety and support:
n
- n
- n
- n
- n Let’s talk about how I can help so you don’t have to drive. I can drive you to get your groceries on Sundays and we can make a day of it!n
- n How do you think those dents got on your car? Are you having trouble with your vision?n
- We’d all feel terrible if you had an accident and got hurt or hurt someone else.
n
n
n
n
n
n
Offer to go for a ride together and then to talk about specific concerns, such as staying in the proper lane, changing lanes, making left-hand turns, speed, or sudden braking. Encourage consideration of a self-evaluation or on-road test, and driving classes to help polish skills.
n
Use examples from familiar experiences. It can be helpful to remind your loved one how his or her parents or grandparents had to cut back on their driving, or how an older neighbor was an unsafe driver.
n
Focus on the risks posed by other drivers. Aggressive or unpredictable drivers can pose more danger to older drivers with slower reaction times.
n
How else can families or friends of older drivers be helpful?
n
- n
- Consider whether to contact their doctor. Ask their doctor if it’s possible to talk with your loved one or friend about their driving. State regulations vary on mandatory reporting of conditions that affect a patient’s ability to drive. Be aware that some doctors may be reluctant to report their patients to their registry of motor vehicles, due to concerns about patient privacy or jeopardizing the patient-doctor relationship.
- Look into rules and regulations around older drivers where your loved one lives. Illinois is currently the only state that requires a road test for older drivers. But many states require vision tests and in-person renewal with increasing frequency for older drivers.
- Consider reporting an unsafe driver to traffic safety authorities. This may feel like a betrayal, but if other efforts have failed this option might be better than waiting until there’s a serious accident.
n
n
n
n
The bottom line
n
In the future, safe, driverless cars may be a solution to the challenge of waning driving skills among older drivers. But we’re not there yet.
n
Right now, we should all acknowledge that it’s not easy to address concerns about impaired older drivers. My best advice is that older drivers and their loved ones try to talk about ways to remain a safe driver and put a plan in place. Ideally, we all would start the conversation well before any driving problems are evident.
n
And it may take more than one conversation. Many more. But let’s face it: sooner or later, most drivers will have to stop driving. For some older drivers, that time may be now. For the rest of us, recognizing this eventuality could help when our time comes.
n “,”excerpt”:”n
Many people experience a decline in their driving skills as they age. While some choose to stop driving, others resist. Whether it’s you or a loved one, planning ahead can help you tackle fixable issues, make transitions easier, and avoid harming yourself or someone else.
n “,”short_excerpt”:”n
Many people experience a decline in their driving skills as they age. While some choose to stop driving, others resist. Whether it’s you or a loved one, planning ahead can help you tackle fixable issues, make transitions easier, and avoid harming yourself or someone else.
n “,”description”:null,”author”:null,”slug”:”what-to-do-when-driving-skills-decline-202311152991″,”sort_date”:”2023-11-15T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2991,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL111523″,”publication_date”:”2023-11-15T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-16T10:00:04.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-11-15T05:00:00.000000Z”,”active”:1,”created_at”:”2023-11-15T10:00:03.000000Z”,”updated_at”:”2023-11-16T10:00:04.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:44,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:23,”cr_id”:2,”featured”:1,”hhp_staff”:1,”hidden”:0,”name”:”Robert H. Shmerling, MD”,”title”:null,”first_name”:”Robert”,”middle_name”:”H.”,”last_name”:”Shmerling”,”suffix”:”MD”,”slug”:”robert-h-shmerling-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing”,”description”:”
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. As a practicing rheumatologist for over 30 years, Dr. Shmerling engaged in a mix of patient care, teaching, and research. His research interests center on diagnostic studies in patients with musculoskeletal symptoms, and rheumatic and autoimmune diseases. He has published research regarding infectious arthritis, medical ethics, and diagnostic test performance in rheumatic disease. Having retired from patient care in 2019, Dr. Shmerling now works as a senior faculty editor for Harvard Health Publishing.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/OdKCKaVzyx3xPsUxIBc9zJz8m3zvysnJa3UJsGOd.jpg”,”twitter_username”:”RobShmerling”,”sort_order”:4,”created_at”:”2021-05-11T10:05:10.000000Z”,”updated_at”:”2023-09-06T15:33:18.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18425,”author_id”:23,”sort_order”:1}}],”contentable”:{“id”:2991,”comments_open”:1,”created_at”:”2023-11-15T10:00:03.000000Z”,”updated_at”:”2023-11-15T10:00:03.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14502,”model_type”:”AppModelsMarketingContent”,”model_id”:18425,”uuid”:”3f091965-a498-4d6a-a299-8fdeeb9dfcfb”,”collection_name”:”contents”,”name”:”bcb42e0d-03e3-4752-8f23-2286f283fb97″,”file_name”:”bcb42e0d-03e3-4752-8f23-2286f283fb97.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:41089,”manipulations”:[],”custom_properties”:{“alt”:”A square-topped gold car key and a gold car on a key ring against a deep yellow background”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14448,”created_at”:”2023-11-15T10:00:03.000000Z”,”updated_at”:”2023-11-15T10:00:04.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14502/bcb42e0d-03e3-4752-8f23-2286f283fb97.jpg”}],”primary_content_topic”:{“id”:44,”name”:”Staying Healthy”,”slug”:”staying-healthy”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/staying-healthy”}},{“id”:18426,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”A tough question: When should an older driver stop driving?”,”short_title”:””,”subheading”:”Be alert to red flags suggesting that a family member — or you — should consider hanging up the keys.”,”summary”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”content”:”
nn  n
n
n
n Part 1 of a two-part series on making decisions about driving as we age. Read Part 2 here. n
n
When my grandmother repeatedly clipped the mailbox backing out of her driveway, she always had a ready explanation: “the sun was in my eyes” or “your grandfather distracted me.” Our family knew we needed to take action. But no one wanted to be the one to ask her to stop driving. She was fiercely independent, didn’t agree that her driving was a problem, and didn’t appreciate our concerns.
n
Maybe there’s a similar story unfolding in your family. Or maybe you’re starting to wonder about your own skills. As part one in a two-part series, this post aims to help people understand red flags to watch for, and why driving abilities change as people age. It also describes a few ways to improve impaired driving, and challenges to navigate.
n
A second post will address ways to strike a balance that respects dignity — and safety — while providing action plans for older drivers and their families.
n
How safe are older drivers on the road?
n
Unsafe drivers can be any age, particularly when drinking is involved. But fatal traffic accidents have risen in both young drivers and older drivers, according to data from the National Safety Council:
n
- n
- Fatalities occurring in crashes involving a driver ages 15 to 20 rose nearly 10% between 2020 and 2021, accounting for 5,565 deaths.
- Among drivers 65 or older, fatalities rose 15% between 2020 and 2021, accounting for more than 8,200 deaths.
n
n
n
While younger drivers may be inexperienced or more likely to be distracted or reckless, older drivers often overestimate their driving abilities. That may be one reason many unsafe older drivers continue to drive despite failing driving skills.
n
Per mile driven, the rate of motor vehicle accidents is higher for drivers ages 80 and older than for almost every other age group, according to the Insurance Institute for Highway Safety. Only the youngest drivers have higher rates. And the rate of fatal motor vehicle accidents per mile driven is higher for drivers aged 85 and older than for every other age group.
n
These statistics reflect the reality that an older driver may not be the only one injured or killed in a crash — occupants in one or more vehicles may be, too. And then there are pedestrians and cyclists at risk.
n
Clearly, the stakes are high when any unsafe driver is on the road. For older drivers with waning driving skills, it’s important to recognize the problem and understand why it’s happening. The following four steps are a good start.
n
1. Seeing any red flags?
n
As people get older, driving skills may decline so slowly that it’s not obvious worrisome changes are happening. Even when mishaps and near-misses occur, there are so many possible contributors —especially other drivers — that it may not be clear that the older driver was at fault.
n
Red flags that might mean an older person is an unsafe driver include:
n
- n
- concerned comments from family or friends
- reluctance of others to ride with them
- input from other drivers (why is everyone honking at me?) or traffic authorities (why am I getting all these traffic tickets?)
- getting lost on familiar roads
- consistently driving too slowly or too fast
- unexplained dents or scratches appearing on the car
- frequent accidents or near-misses.
n
n
n
n
n
n
n
n
2. Why do driving skills tend to wane with age?
n
While people of advanced age can safely drive (and many do!), driving skills may wane due to:
n
- n
- medical conditions, such as arthritis, neuropathy, or dementia
- medications, such as sedatives or certain antidepressants
- age-related changes in reaction time
- trouble with vision or hearing
- other physical changes related to aging, such as less flexibility or strength
- difficulty processing rapidly changing information. For example, an older driver may be more likely than a younger driver to accidentally press the gas pedal instead of the brake when needing to stop suddenly.
n
n
n
n
n
n
n
3. What can — and can’t — be reversed to improve driving?
n
Some changes that impair driving can be reversed or a workaround can be found. For example, if driving is impaired due to cataracts, cataract surgery can restore vision and improve driving. If night driving is difficult, it’s best to drive only during the day. If memory problems are starting to arise, it may still be possible to drive safely in more limited circumstances.
n
Driving problems due to advanced dementia or a major stroke affecting judgment and physical skills are much less likely to improve.
n
4. Accept that conversations about not driving are challenging
n
If there is no simple way to reverse or work around declining driving skills, accept that there will be many challenges to navigate, whether you’re the older driver or a family member.
n
Challenges facing the driver:
n
- n
- It’s not easy to acknowledge declining function. Driving impairment is an unsettling milestone, an indication that the future may include further loss of abilities.
- It can feel unnecessary and unreasonable. Most older folks facing a decision about whether it’s safe to continue driving were good drivers not so long ago. They may still see themselves as competent drivers, and see efforts to restrict their driving as overly cautious or demeaning.
- Denial and defensiveness are common. Even when all the signs are there, it may be tempting for a poor driver to deflect blame (for example, blaming other drivers).
- Not driving is a loss of independence. Sure, there are other ways to get around and nondrivers can certainly be independent. But few alternatives rival the independence that comes with being able to drive yourself. And, depending on where you live, public transportation or other alternatives to driving may be limited.
n
n
n
n
n
Challenges facing the family:
n
- n
- Often, the older driver doesn’t share their family’s concerns about driving safety. This can lead to arguments, confrontation, and resentment.
- The safety of others is at stake. The older driver with waning skills may endanger many people besides themselves: passengers in their care, other drivers and their passengers, cyclists, and pedestrians.
- It’s hard to know when the time is right. Speaking up too soon may lead to unnecessary restrictions on a loved one’s favored means of transportation, not to mention family strife. Waiting too long can lead to avoidable tragedy.
n
n
n
n
Finding a path forward
n
As for my grandmother, none of us knew what to say. Should we try to get her to agree to stop driving entirely or let her ease into the idea over time? Maybe she could stop driving at night or limit her driving to short distances. Should we bring it to the attention of her doctor and let them direct the next steps? Or should we take an even harder step and report her to the authorities?
n
If you’re asking similar questions — or if you’re starting to wonder about your own driving abilities — you may feel strongly that it’s important to respect individual preferences, dignity, and independence. Yet you also want to protect everyone from harm.
n
What are the best ways to strike a balance? Can you test and improve how an older driver is doing behind the wheel? Can you navigate tough conversations in ways that allow room for both independence and safety? These are the subjects to be tackled in Part 2.
n “,”excerpt”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”short_excerpt”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”description”:null,”author”:null,”slug”:”a-tough-question-when-should-an-older-driver-stop-driving-202311132992″,”sort_date”:”2023-11-13T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2992,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL111323″,”publication_date”:”2023-11-13T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-16T10:00:03.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-11-15T05:00:00.000000Z”,”active”:1,”created_at”:”2023-11-15T21:34:38.000000Z”,”updated_at”:”2023-11-16T10:00:03.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:44,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:23,”cr_id”:2,”featured”:1,”hhp_staff”:1,”hidden”:0,”name”:”Robert H. Shmerling, MD”,”title”:null,”first_name”:”Robert”,”middle_name”:”H.”,”last_name”:”Shmerling”,”suffix”:”MD”,”slug”:”robert-h-shmerling-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing”,”description”:”
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. As a practicing rheumatologist for over 30 years, Dr. Shmerling engaged in a mix of patient care, teaching, and research. His research interests center on diagnostic studies in patients with musculoskeletal symptoms, and rheumatic and autoimmune diseases. He has published research regarding infectious arthritis, medical ethics, and diagnostic test performance in rheumatic disease. Having retired from patient care in 2019, Dr. Shmerling now works as a senior faculty editor for Harvard Health Publishing.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/OdKCKaVzyx3xPsUxIBc9zJz8m3zvysnJa3UJsGOd.jpg”,”twitter_username”:”RobShmerling”,”sort_order”:4,”created_at”:”2021-05-11T10:05:10.000000Z”,”updated_at”:”2023-09-06T15:33:18.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18426,”author_id”:23,”sort_order”:1}}],”contentable”:{“id”:2992,”comments_open”:1,”created_at”:”2023-11-15T21:34:38.000000Z”,”updated_at”:”2023-11-15T21:34:38.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14503,”model_type”:”AppModelsMarketingContent”,”model_id”:18426,”uuid”:”253e11aa-2393-4c3c-af23-b812d32e9c0c”,”collection_name”:”contents”,”name”:”f6fd51a8-b6bf-4a40-9b61-0067cf611802″,”file_name”:”f6fd51a8-b6bf-4a40-9b61-0067cf611802.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:70537,”manipulations”:[],”custom_properties”:{“alt”:”Abstract of traffic on city highway at night with glaring headlights forming big, colored dots “},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14449,”created_at”:”2023-11-15T21:34:38.000000Z”,”updated_at”:”2023-11-15T21:34:41.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14503/f6fd51a8-b6bf-4a40-9b61-0067cf611802.jpg”}],”primary_content_topic”:{“id”:44,”name”:”Staying Healthy”,”slug”:”staying-healthy”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/staying-healthy”}},{“id”:18427,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”A tough question: When should an older driver stop driving?”,”short_title”:””,”subheading”:”Be alert to red flags suggesting that a family member – or you –– should consider hanging up the keys.”,”summary”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”content”:”
n  n
n
n
n Part 1 of a two-part series on making decisions about driving as we age. Read Part 2 here. n
n
When my grandmother repeatedly clipped the mailbox backing out of her driveway, she always had a ready explanation: “the sun was in my eyes” or “your grandfather distracted me.” Our family knew we needed to take action. But no one wanted to be the one to ask her to stop driving. She was fiercely independent, didn’t agree that her driving was a problem, and didn’t appreciate our concerns.
n
Maybe there’s a similar story unfolding in your family. Or maybe you’re starting to wonder about your own skills. As part one in a two-part series, this post aims to help people understand red flags to watch for, and why driving abilities change as people age. It also describes a few ways to improve impaired driving, and challenges to navigate.
n
A second post will address ways to strike a balance that respects dignity — and safety — while providing action plans for older drivers and their families.
n
How safe are older drivers on the road?
n
Unsafe drivers can be any age, particularly when drinking is involved. But fatal traffic accidents have risen in both young drivers and older drivers, according to data from the National Safety Council:
n
- n
- Fatalities occurring in crashes involving a driver ages 15 to 20 rose nearly 10% between 2020 and 2021, accounting for 5,565 deaths.
- Among drivers 65 or older, fatalities rose 15% between 2020 and 2021, accounting for more than 8,200 deaths.
n
n
n
While younger drivers may be inexperienced or more likely to be distracted or reckless, older drivers often overestimate their driving abilities. That may be one reason many unsafe older drivers continue to drive despite failing driving skills.
n
Per mile driven, the rate of motor vehicle accidents is higher for drivers ages 80 and older than for almost every other age group, according to the Insurance Institute for Highway Safety. Only the youngest drivers have higher rates. And the rate of fatal motor vehicle accidents per mile driven is higher for drivers aged 85 and older than for every other age group.
n
These statistics reflect the reality that an older driver may not be the only one injured or killed in a crash — occupants in one or more vehicles may be, too. And then there are pedestrians and cyclists at risk.
n
Clearly, the stakes are high when any unsafe driver is on the road. For older drivers with waning driving skills, it’s important to recognize the problem and understand why it’s happening. The following four steps are a good start.
n
1. Seeing any red flags?
n
As people get older, driving skills may decline so slowly that it’s not obvious worrisome changes are happening. Even when mishaps and near-misses occur, there are so many possible contributors —especially other drivers — that it may not be clear that the older driver was at fault.
n
Red flags that might mean an older person is an unsafe driver include:
n
- n
- concerned comments from family or friends
- reluctance of others to ride with them
- input from other drivers (why is everyone honking at me?) or traffic authorities (why am I getting all these traffic tickets?)
- getting lost on familiar roads
- consistently driving too slowly or too fast
- unexplained dents or scratches appearing on the car
- frequent accidents or near-misses.
n
n
n
n
n
n
n
n
2. Why do driving skills tend to wane with age?
n
While people of advanced age can safely drive (and many do!), driving skills may wane due to:
n
- n
- medical conditions, such as arthritis, neuropathy, or dementia
- medications, such as sedatives or certain antidepressants
- age-related changes in reaction time
- trouble with vision or hearing
- other physical changes related to aging, such as less flexibility or strength
- difficulty processing rapidly changing information. For example, an older driver may be more likely than a younger driver to accidentally press the gas pedal instead of the brake when needing to stop suddenly.
n
n
n
n
n
n
n
3. What can — and can’t — be reversed to improve driving?
n
Some changes that impair driving can be reversed or a workaround can be found. For example, if driving is impaired due to cataracts, cataract surgery can restore vision and improve driving. If night driving is difficult, it’s best to drive only during the day. If memory problems are starting to arise, it may still be possible to drive safely in more limited circumstances.
n
Driving problems due to advanced dementia or a major stroke affecting judgment and physical skills are much less likely to improve.
n
4. Accept that conversations about not driving are challenging
n
If there is no simple way to reverse or work around declining driving skills, accept that there will be many challenges to navigate, whether you’re the older driver or a family member.
n
Challenges facing the driver:
n
- n
- It’s not easy to acknowledge declining function. Driving impairment is an unsettling milestone, an indication that the future may include further loss of abilities.
- It can feel unnecessary and unreasonable. Most older folks facing a decision about whether it’s safe to continue driving were good drivers not so long ago. They may still see themselves as competent drivers, and see efforts to restrict their driving as overly cautious or demeaning.
- Denial and defensiveness are common. Even when all the signs are there, it may be tempting for a poor driver to deflect blame (for example, blaming other drivers).
- Not driving is a loss of independence. Sure, there are other ways to get around and nondrivers can certainly be independent. But few alternatives rival the independence that comes with being able to drive yourself. And, depending on where you live, public transportation or other alternatives to driving may be limited.
n
n
n
n
n
Challenges facing the family:
n
- n
- Often, the older driver doesn’t share their family’s concerns about driving safety. This can lead to arguments, confrontation, and resentment.
- The safety of others is at stake. The older driver with waning skills may endanger many people besides themselves: passengers in their care, other drivers and their passengers, cyclists, and pedestrians.
- It’s hard to know when the time is right. Speaking up too soon may lead to unnecessary restrictions on a loved one’s favored means of transportation, not to mention family strife. Waiting too long can lead to avoidable tragedy.
n
n
n
n
Finding a path forward
n
As for my grandmother, none of us knew what to say. Should we try to get her to agree to stop driving entirely or let her ease into the idea over time? Maybe she could stop driving at night or limit her driving to short distances. Should we bring it to the attention of her doctor and let them direct the next steps? Or should we take an even harder step and report her to the authorities?
n
If you’re asking similar questions — or if you’re starting to wonder about your own driving abilities — you may feel strongly that it’s important to respect individual preferences, dignity, and independence. Yet you also want to protect everyone from harm.
n
What are the best ways to strike a balance? Can you test and improve how an older driver is doing behind the wheel? Can you navigate tough conversations in ways that allow room for both independence and safety? These are the subjects to be tackled in Part 2.
“,”excerpt”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”short_excerpt”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”description”:null,”author”:null,”slug”:”a-tough-question-when-should-an-older-driver-stop-driving-202311132993″,”sort_date”:”2023-11-13T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2993,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL11132023″,”publication_date”:”2023-11-13T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-16T10:00:05.000000Z”,”last_import_type”:”insert”,”last_modified_date”:”2023-11-15T05:00:00.000000Z”,”active”:1,”created_at”:”2023-11-16T10:00:05.000000Z”,”updated_at”:”2023-11-16T10:00:05.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:44,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:23,”cr_id”:2,”featured”:1,”hhp_staff”:1,”hidden”:0,”name”:”Robert H. Shmerling, MD”,”title”:null,”first_name”:”Robert”,”middle_name”:”H.”,”last_name”:”Shmerling”,”suffix”:”MD”,”slug”:”robert-h-shmerling-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing”,”description”:”
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. As a practicing rheumatologist for over 30 years, Dr. Shmerling engaged in a mix of patient care, teaching, and research. His research interests center on diagnostic studies in patients with musculoskeletal symptoms, and rheumatic and autoimmune diseases. He has published research regarding infectious arthritis, medical ethics, and diagnostic test performance in rheumatic disease. Having retired from patient care in 2019, Dr. Shmerling now works as a senior faculty editor for Harvard Health Publishing.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/OdKCKaVzyx3xPsUxIBc9zJz8m3zvysnJa3UJsGOd.jpg”,”twitter_username”:”RobShmerling”,”sort_order”:4,”created_at”:”2021-05-11T10:05:10.000000Z”,”updated_at”:”2023-09-06T15:33:18.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18427,”author_id”:23,”sort_order”:1}}],”contentable”:{“id”:2993,”comments_open”:1,”created_at”:”2023-11-16T10:00:05.000000Z”,”updated_at”:”2023-11-16T10:00:05.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14504,”model_type”:”AppModelsMarketingContent”,”model_id”:18427,”uuid”:”3b34d315-4952-4834-b625-2ad8ce40b497″,”collection_name”:”contents”,”name”:”f6fd51a8-b6bf-4a40-9b61-0067cf611802″,”file_name”:”f6fd51a8-b6bf-4a40-9b61-0067cf611802.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:70537,”manipulations”:[],”custom_properties”:{“alt”:”Abstract of traffic on city highway at night with glaring headlights forming big, colored dots “},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14450,”created_at”:”2023-11-16T10:00:05.000000Z”,”updated_at”:”2023-11-16T10:00:06.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14504/f6fd51a8-b6bf-4a40-9b61-0067cf611802.jpg”}],”primary_content_topic”:{“id”:44,”name”:”Staying Healthy”,”slug”:”staying-healthy”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/staying-healthy”}},{“id”:17918,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”3 ways to create community and counter loneliness”,”short_title”:””,”subheading”:”Breaking through loneliness to build connections and enhance well-being.”,”summary”:”n
Loneliness boosts risk for many health problems, and can even contribute to an early death. Many people find it hard to reach out to make new friends, but there are strategies that can help.
n “,”content”:”
nn  n
n
n
Loneliness is complicated. You can feel lonely when you lack friends and miss companionship, or when you’re surrounded by people — even friends and family.
n
Either way, loneliness can have devastating health effects. It boosts risk for coronary artery disease, stroke, depression, high blood pressure, declining thinking skills, inability to perform daily living tasks, and even an early death. The remedy? Below we offer three ways to ease loneliness and add happiness by helping you expand your social network.
n
Taking the first steps
n
Not all loneliness can be solved by seeking out people. Loneliness that occurs despite relationships may require talk therapy and a journey that looks inward.
n
Reducing loneliness caused by a lack of relationships is more of an outward journey to make new friends. “That’s a challenge as we get older, because people are often established in their social groups and aren’t as available as they might have been in a different phase of life. So you have to be more entrepreneurial and work harder to make friends than you once did,” says Dr. Jacqueline Olds, a psychiatrist at Harvard-affiliated McLean Hospital and the coauthor of two books on loneliness.
n
Trying these strategies can help.
n
1. Seek like-minded souls
n
Being around people who share your interests gives you a head start on making friends: you already have something in common.
n
Start by considering your interests. Are you a voracious reader, a history lover, a movie aficionado, a gardener, a foodie, a puppy parent, or an athlete? Are you passionate about a cause, your community, or your heritage? Do you collect things? Do you love classic cars? Do you enjoy sprucing up old furniture? Maybe you want to learn something new, like how to cook Chinese food or speak another language. Search for online groups, in-person clubs, volunteer opportunities, or classes that match any of your interests or things you’d like to try.
n
Once you join a group, you’ll need to take part in it regularly to build bonds. If you can gather in person, it’s even better. “The part of our brain involved in social connection is stimulated by all five senses. When you’re with someone in the same room, you get a much stronger set of stimuli than you do by watching them on an electronic screen,” Dr. Olds says.
n
2. Create opportunities
n
If joining someone else’s group is unappealing, start your own. Host gatherings at your place or elsewhere. “All it takes is three people. You can say, ‘Let’s read books or talk about a TV show or have a dinner group on a regular basis,'” Dr. Olds says.
n
Other ideas for gatherings — either weekly or monthly — include:
n
- n
- game nights
- trivia nights
- hikes in interesting parks
- beach walks
- bird-watching expeditions
- running or cycling
- n meditationn
- museum visits
- cooking
- knitting, sewing, or crafting
- shopping
- day trips to nearby towns
- jewelry making
- collector show-and-tell (comic books, antique dolls, baseball cards).
n
n
n
n
n
n
n
n
n
n
n
n
n
n
n
The people you invite don’t have to be dear friends; they can just be people you’d like to get to know better — perhaps neighbors or work acquaintances.
n
If they’re interested in a regular gathering, pin down dates and times. Otherwise, the idea might stay stuck in the talking stages. “Don’t be timid. Say, ‘Let’s get our calendars out and get this scheduled,'” Dr. Olds says.
n
3. Brush up your social skills
n
Sometimes we’re rusty in surface social graces that help build deeper connections. “It makes a huge difference when you can be enthusiastic rather than just sitting there and hoping someone will realize how interesting you are,” Dr. Olds says.
n
Tips to practice:
n
- n
- Smile more. Smiling is welcoming, inviting, and hospitable to others.
- Be engaging. Prepare a few topics to talk about or questions to ask — perhaps about the news or the reason you’ve gathered (if it’s a seminar, for example, ask how long someone has been interested in the subject). Or look for a conversation starter. “Maybe the person is wearing a pretty brooch. Ask if there’s a story behind it,” Dr. Olds suggests.
- Be a good listener. “Listen in a way that someone realizes you’re paying attention. Hold their gaze, nod your head or say ‘Mm hmm’ as they’re talking so you give feedback. Assume everyone in the world is just yearning for your feedback,” Dr. Olds says.
- Ask follow-up questions. Don’t ignore signals that someone has interesting stories to tell. “If they allude to something, your job is to look fascinated and ask if they can tell you more. They’re dropping crumbs on a path to a deeper exchange,” Dr. Olds notes.
n
n
n
n
n
Even chats that don’t lead to friendships can be enriching. A 2022 study found that people who had the most diverse portfolios of social interactions — exchanges with strangers, acquaintances, friends, or family members — were much happier than those with the least diverse social portfolios.
n
Ultimately, a wide variety of interactions contributes to well-being, whether you’re talking to the cashier at the supermarket, a neighbor, an old friend, or a new one. And all of these connections combined may go a long way toward helping you feel less lonely.
n “,”excerpt”:”n
Loneliness boosts risk for many health problems, and can even contribute to an early death. Many people find it hard to reach out to make new friends, but there are strategies that can help.
n “,”short_excerpt”:”n
Loneliness boosts risk for many health problems, and can even contribute to an early death. Many people find it hard to reach out to make new friends, but there are strategies that can help.
n “,”description”:null,”author”:null,”slug”:”3-ways-to-create-community-and-counter-loneliness-202303082900″,”sort_date”:”2023-03-08T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2900,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”Bl030823″,”publication_date”:”2023-03-08T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-04-23T09:00:13.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-04-22T04:00:00.000000Z”,”active”:1,”created_at”:”2023-03-08T10:00:02.000000Z”,”updated_at”:”2023-04-23T09:00:13.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:37,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:31,”cr_id”:117,”featured”:0,”hhp_staff”:0,”hidden”:0,”name”:”Heidi Godman”,”title”:null,”first_name”:”Heidi”,”middle_name”:null,”last_name”:”Godman”,”suffix”:null,”slug”:”heidi-godman”,”byline”:”Executive Editor, Harvard Health Letter“,”description”:”
Heidi Godman is the executive editor of the Harvard Health Letter. Before coming to the Health Letter, she was an award-winning television news anchor and medical reporter for 25 years. Heidi was named a journalism fellow of the American Academy of Neurology, and has been honored by the Associated Press, the American Heart Association, the Wellness Community, and other organizations for outstanding medical reporting. Heidi holds a bachelor of science degree in journalism from West Virginia University.
“,”image_url”:”https://hohmature.news/wp-content/uploads/2023/09/jmHxTqYhe8m1bTrPQJnvY8odf8gsq1y1Q0i6Wp6Y.jpg”,”twitter_username”:null,”sort_order”:0,”created_at”:”2021-05-11T10:08:08.000000Z”,”updated_at”:”2022-08-03T17:04:41.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:17918,”author_id”:31,”sort_order”:1}}],”contentable”:{“id”:2900,”comments_open”:1,”created_at”:”2023-03-08T10:00:02.000000Z”,”updated_at”:”2023-04-13T15:22:45.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:13637,”model_type”:”AppModelsMarketingContent”,”model_id”:17918,”uuid”:”0af6ca4e-a1ee-4a7b-b9fb-a538b7d94695″,”collection_name”:”contents”,”name”:”24b364ff-eead-4160-9c1a-13890a2a4ad2″,”file_name”:”24b364ff-eead-4160-9c1a-13890a2a4ad2.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:283380,”manipulations”:[],”custom_properties”:{“alt”:”A high, overhead view looking down on a large crowd of tiny people and one tiny person standing alone in an empty, white, heart-shaped space “},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:13600,”created_at”:”2023-03-08T10:00:02.000000Z”,”updated_at”:”2023-03-08T10:00:11.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/13637/24b364ff-eead-4160-9c1a-13890a2a4ad2.jpg”}],”primary_content_topic”:{“id”:37,”name”:”Mind & Mood”,”slug”:”mind-and-mood”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/mind-and-mood”}},{“id”:18419,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Opill: Is this new birth control pill right for you?”,”short_title”:””,”subheading”:”Answers to key questions about the over-the-counter birth control pill approved by the FDA.”,”summary”:”n
The first nonprescription daily oral contraceptive was approved by the FDA earlier this year. Opill is expected to be available in early 2024. Here's what you should know about this new birth control pill.
n “,”content”:”
nn  n
n
n
Birth control pills have been safely used in the US (and sold only by prescription) for more than half a century. Just this past summer, the FDA approved Opill, the first daily contraceptive pill intended for sale over the counter. This offers many more people access to a new nonprescription option for preventing pregnancy.
n
Opill may be available early in 2024, although the exact date and cost are not yet known. Here’s what anyone interested — adults, parents, and teens — should know.
n
What is in Opill and how does it work?
n
Opill is a progestin-only form of birth control. That means it uses a single hormone called progestin (or norgestrel) to prevent pregnancy. It works by
n
- n
- affecting ovulation so that the ovaries do not release an egg every month
- thickening cervical mucus, which blocks sperm from reaching an egg
- changing the uterine lining in ways that keep a fertilized egg from implanting.
n
n
n
n
How effective is Opill at preventing pregnancy?
n
It depends on how consistent you are about taking Opill:
n
- n
- Perfect use means taking the pill every single day at the same time. With perfect use, Opill is 98% effective. That means that if 100 people take the medication perfectly, two or fewer people would become pregnant. Taking a pill perfectly can be difficult, though.
- Typical use averages how well a method works to prevent pregnancy when real people use it in real life. It considers that people sometimes use the pill inconsistently, like forgetting a dose or not taking it at the same time every day. With typical use, Opill is 91% effective. This means that if 100 people use Opill, but don’t take it perfectly, at least nine could become pregnant in a year.
n
n
n
It's also important to know that some medications make Opill less effective at preventing pregnancy. These include medicines used to treat migraines and seizures. Even though this birth control pill will be available over the counter, you should ask your health care provider if any medicines you take could make it less effective.
n
How do you take Opill?
n
- n
- Take it once a day at the same time each day until you finish the entire pack.
- Sticking to a consistent time of day, every day, is crucial. Timing matters with progestin-only pills like Opill because this medication works by raising progestin levels. However, progestin only stays elevated for 24 hours after you take each pill. After that, the progestin level will return to normal.
- After you complete a 28-day pack, you should immediately start a new pack of pills the next day.
n
n
n
n
What happens if you forget to take a dose at the specific time or miss a dose?
n
- n
- If you take the pill more than three hours late it will not be as effective at preventing pregnancy.
- Take the missed pill as soon you remember.
- You will need to use a backup birth control method such as condoms every time you have sex for the next 48 hours.
n
n
n
n
Is Opill safe for teenagers?
n
Opill is generally safe for most people who could get pregnant, including teenagers. There’s no evidence to suggest that safety or side effects are different in teenagers compared with adults.
n
Research done by the manufacturer has established the safety of Opill in people as young as 15 years old. It will be available without an age restriction.
n
When teens use birth control, what is the best choice for them?
n
There isn't a one-size-fits-all birth control method for all teenagers. The best method is the one a teen personally prefers and is committed to using consistently.
n
For teens who struggle with taking medication at the same time every day –– or anyone else who does –– Opill may not be the right choice. Fortunately, there are many options for preventing pregnancy, catering to individual preferences and goals.
n
Learn more about different contraception methods at the Center for Young Women’s Health website.
n
What side effects are common with Opill?
n
Progestin-only pills are usually associated with mild side effects. The most common side effects are:
n
- n
- unexpected vaginal bleeding or spotting
- acne
- headache
- gastrointestinal symptoms such as nausea, abdominal pain, and bloating
- change in appetite.
n
n
n
n
n
n
Opill does not cause problems with getting pregnant in the future, or cause cancer. Unlike birth control pills that combine the hormones estrogen and progestin, Opill will not increase the risk of a developing a blood clot.
n
Will Opill cause any mood changes?
n
Research looking at possible effects of progestin-only pills on mood is limited, so this is unclear. We do know that most people who take hormonal birth control methods do not experience negative mood changes.
n
Fortunately, there are many different types of effective birth control. If one method causes you unwanted side effects, talk to your health care provider. Together, you can figure out if another type of birth control may work better for you.
n
Can it be used as emergency birth control?
n
No, it should not be used as emergency birth control.
n
What should you know about STIs?
n
This type of birth control does not protect you from sexually transmitted infections (STIs) such as syphilis, gonorrhea, or chlamydia.
n
You can reduce the chance of getting STIs by correctly using condoms each time you have sex. There are different types of condoms: one made for penises and one made for vaginas.
n
Vaccines help protect against some STIs such as hepatitis B and human papillomavirus (HPV). A medicine called PrEP can help prevent HIV. Ask your medical team for more information about the right choices for you.
n
When will Opill be available and what will it cost?
n
The timeline for availability and the cost of medication is determined by the manufacturer. At time of FDA approval, it was expected to hit shelves in early 2024. No updates have been released for the exact date or estimated cost of the medication.
n “,”excerpt”:”n
The first nonprescription daily oral contraceptive was approved by the FDA earlier this year. Opill is expected to be available in early 2024. Here's what you should know about this new birth control pill.
n “,”short_excerpt”:”n
The first nonprescription daily oral contraceptive was approved by the FDA earlier this year. Opill is expected to be available in early 2024. Here's what you should know about this new birth control pill.
n “,”description”:null,”author”:null,”slug”:”opill-is-this-new-birth-control-pill-right-for-you-202311082989″,”sort_date”:”2023-11-08T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2989,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL110823″,”publication_date”:”2023-11-08T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-14T10:00:04.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-11-13T05:00:00.000000Z”,”active”:1,”created_at”:”2023-11-07T10:00:03.000000Z”,”updated_at”:”2023-11-14T10:00:04.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:46,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:474,”cr_id”:838,”featured”:0,”hhp_staff”:0,”hidden”:0,”name”:”Candice Mazon, MD”,”title”:null,”first_name”:”Candice”,”middle_name”:null,”last_name”:”Mazon”,”suffix”:”MD”,”slug”:”candice-mazon-md”,”byline”:”Contributor”,”description”:”
Dr. Candice Mazon is a second year adolescent medicine fellow at Boston Children's Hospital. She's a board certified pediatrician and received her training at MedStar Georgetown University Hospital. She earned her MD degree from Drexel University College of Medicine. Her interests include sexual health and reproductive justice, as well as addressing various health inequities.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/Ogerjm1yqEC3aCY8XysGOCpPbwDaK88HqOFofwog.jpg”,”twitter_username”:null,”sort_order”:0,”created_at”:”2023-11-06T18:45:44.000000Z”,”updated_at”:”2023-11-06T18:45:44.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18419,”author_id”:474,”sort_order”:1}},{“id”:475,”cr_id”:839,”featured”:0,”hhp_staff”:0,”hidden”:0,”name”:”Amy Desrochers DiVasta, MD, MMSc”,”title”:null,”first_name”:”Amy”,”middle_name”:”Desrochers”,”last_name”:”DiVasta”,”suffix”:”MD, MMSc”,”slug”:”amy-desrochers-divasta-md-mmsc”,”byline”:”Contributor”,”description”:”
Amy Desrochers DiVasta MD, MMSc, is chief of the division of adolescent medicine at Boston Children’s Hospital. She is the co-director of the adolescent long-acting reversible contraception program, and co-director of the reproductive endocrinology and PCOS program. Dr. DiVasta's research interests include the bone health of young women with low-estrogen states, such as girls with eating disorders, as well as reproductive health issues including long-acting contraception, PCOS, and endometriosis.
rnrn
Dr. DiVasta is also the co-scientific director for the Boston Center for Endometriosis, a joint project between Boston Children’s Hospital and Brigham and Women’s Hospital.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/nNkjO4OxGB16pAl5q3sHq30Cdje2Vy2mCA0a8N42.gif”,”twitter_username”:null,”sort_order”:0,”created_at”:”2023-11-06T22:06:13.000000Z”,”updated_at”:”2023-11-06T22:06:13.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18419,”author_id”:475,”sort_order”:2}}],”contentable”:{“id”:2989,”comments_open”:1,”created_at”:”2023-11-07T10:00:03.000000Z”,”updated_at”:”2023-11-07T10:00:03.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14494,”model_type”:”AppModelsMarketingContent”,”model_id”:18419,”uuid”:”7c0d1044-f18c-4f74-838c-4eecc2881928″,”collection_name”:”contents”,”name”:”ec54ca7d-b745-4ffb-8cf1-2b5ea1d438dd”,”file_name”:”ec54ca7d-b745-4ffb-8cf1-2b5ea1d438dd.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:122412,”manipulations”:[],”custom_properties”:{“alt”:”photo of a silver blister pack of birth control pills with the four rows of days of the week”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14440,”created_at”:”2023-11-07T10:00:03.000000Z”,”updated_at”:”2023-11-07T10:00:06.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14494/ec54ca7d-b745-4ffb-8cf1-2b5ea1d438dd.jpg”}],”primary_content_topic”:{“id”:46,”name”:”Women’s Health”,”slug”:”womens-health”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/womens-health”}},{“id”:18417,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Do children get migraine headaches? What parents need to know”,”short_title”:null,”subheading”:”A throbbing headache, nausea, and light sensitivity may be symptoms of migraine in children and teens”,”summary”:”
Headaches are very common in children and teens. We don’t tend to think about children getting migraines, but by age 10 one in 20 children has had one. Symptoms may differ from adults and it’s important for parents to understand triggers, helpful treatments, and possible red flags.
“,”content”:”

rnrn
Headaches are very common in children and teens. In fact, more than half will suffer from headaches at some point, and by 18 years the majority of adolescents have had them. And while most headaches are part of a viral illness, some are migraines. In fact, recurring migraines affect as many as one in 10 children and teens overall.
rnrn
What should you know — and do — if you think your child or teen may be having migraines?
rnrn
How early do migraines start to occur?
rnrn
We don't tend to think about migraines in children, but by age 10, one in 20 children has had a migraine. And migraines sometimes occur even earlier.
rnrn
Before puberty, boys and girls are equally likely to have them. After puberty, migraines are more common in girls.
rnrn
Which migraine symptoms are most common in children?
rnrn
Migraines are often one-sided in adults. In children they are more likely to be felt on both sides of the head, either in both temples or both sides of the forehead.
rnrn
While it's not always easy to tell a migraine from another kind of headache, children
rnrn
- rnt
- often report throbbing pain
- may experience nausea and sensitivity to light and noise.
rnt
rn
rnrn
The flashing lights and other vision changes people often see as a migraine begins are less common in children. However, parents may notice that their child is more tired, irritable, or pale before a migraine begins — and takes a while to get back to normal after it ends.
rnrn
What causes migraines in children?
rnrn
We don't know exactly what causes migraines. We used to think it had to do with blood flow to the brain, but that does not seem to be the case. It appears that migraines are caused by the nerves being more sensitive, and more reactive to stimulation. That stimulation could be stress, fatigue, hunger, almost anything.
rnrn
Migraines run in families. In fact, most migraine sufferers have someone in the family who gets migraines too.
rnrn
Can migraines be prevented?
rnrn
The best way to prevent migraines is to identify and avoid triggers. The triggers are different in each person, which is why it's a good idea to keep a headache diary.
rnrn
When your child gets a headache, write down what was happening before the headache, how badly it hurt and where, what helped, and anything else about it you can think of. This helps you and your doctor see patterns that can help you understand your child's particular triggers.
rnrn
It's a good idea to make sure your child gets enough sleep, eats regularly and healthfully, drinks water regularly, gets exercise, and manages stress. Doing this not only helps prevent migraines, but is also good for overall health!
rnrn
How can you help your child ease a migraine?
rnrn
When a migraine strikes, sometimes just lying down in a dark, quiet room with a cool cloth on the forehead is enough. If it's not, ibuprofen or acetaminophen can be helpful; your doctor can tell you the best dose for your child.
rnrn
It's important not to give your child these medications more than about 14 days a month, as giving them more often can lead to rebound headaches and make everything worse!
rnrn
Are there prescription medicines that can help children with migraines?
rnrn
If those approaches aren't enough, a class of medications called triptans can be helpful in stopping migraines in children ages 6 and up.
rnrn
If a child experiences frequent or severe migraines, leading to missed days of school or otherwise interfering with life, doctors often use medications to prevent migraines. There are a number of different kinds, and your doctor can advise you on what would be best for your child.
rnrn
Some girls get migraines around the time of their period. If that happens frequently, sometimes taking a prevention medicine around the time of menses each month can be helpful.
rnrn
When to contact your doctor
rnrn
If you think your child might be having migraines, you should call and make an appointment. Bring the headache diary with you. Your doctor will ask a bunch of questions, do a physical examination, and make a diagnosis. Together you can come up with the best plan for your child.
rnrn
You should always call your doctor, or go to an emergency room, if your child has a severe headache, a stiff neck, trouble with coordination or movement, is abnormally sleepy, or isn't talking or behaving normally.
rnrn
The American Academy of Pediatrics has additional useful information about migraines, and how to treat and prevent them, on their website.
“,”excerpt”:”
Headaches are very common in children and teens. We don’t tend to think about children getting migraines, but by age 10 one in 20 children has had one. Symptoms may differ from adults and it’s important for parents to understand triggers, helpful treatments, and possible red flags.
“,”short_excerpt”:”n
Headaches are very common in children and teens. We don’t tend to think about children getting migraines, but by age 10 one in 20 children has had one. Symptoms may differ from adults and it’s important for parents to understand triggers, helpful treatments, and possible red flags.
n “,”description”:null,”author”:null,”slug”:”do-children-get-migraine-headaches-what-parents-need-to-know-202311062988″,”sort_date”:”2023-11-06T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2988,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL110623″,”publication_date”:”2023-11-06T05:00:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-06T05:00:00.000000Z”,”last_import_type”:”insert”,”last_modified_date”:”2023-11-05T04:00:00.000000Z”,”active”:1,”created_at”:”2023-11-06T10:00:03.000000Z”,”updated_at”:”2023-11-08T21:43:11.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:24,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:46,”cr_id”:4,”featured”:0,”hhp_staff”:1,”hidden”:0,”name”:”Claire McCarthy, MD”,”title”:null,”first_name”:”Claire”,”middle_name”:null,”last_name”:”McCarthy”,”suffix”:”MD”,”slug”:”claire-mccarthy-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing”,”description”:”Claire McCarthy, MD, is a primary care pediatrician at Boston Children’s Hospital, and an assistant professor of pediatrics at Harvard Medical School. In addition to being a senior faculty editor for Harvard Health Publishing, Dr. McCarthy writes about health and parenting for Boston Children’s Hospital, Boston.com, and the Huffington Post.”,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/mvCBqecmOmDXOhy74hH3DviJmMAprZqhFgGbhTJL.jpg”,”twitter_username”:null,”sort_order”:5,”created_at”:”2021-05-11T10:23:17.000000Z”,”updated_at”:”2023-09-05T22:36:44.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18417,”author_id”:46,”sort_order”:1}}],”contentable”:{“id”:2988,”comments_open”:1,”created_at”:”2023-11-06T10:00:03.000000Z”,”updated_at”:”2023-11-08T21:43:11.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14489,”model_type”:”AppModelsMarketingContent”,”model_id”:18417,”uuid”:”af718b0f-65b7-4fc5-bd44-c8b03de827c8″,”collection_name”:”contents”,”name”:”cf914d00-e65a-4a1f-9d1d-146785bd94b1″,”file_name”:”cf914d00-e65a-4a1f-9d1d-146785bd94b1.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:90345,”manipulations”:[],”custom_properties”:{“alt”:”Brown-haired boy lying on colorful spread, looks pained, one hand covering an eye, other eye shut & other hand tucked behind head; concept is migraine headache”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14435,”created_at”:”2023-11-06T10:00:03.000000Z”,”updated_at”:”2023-11-06T10:00:12.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14489/cf914d00-e65a-4a1f-9d1d-146785bd94b1.jpg”}],”primary_content_topic”:{“id”:24,”name”:”Child & Teen Health”,”slug”:”child-and-teen-health”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/child-and-teen-health”}},{“id”:18039,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Does running cause arthritis?”,”short_title”:””,”subheading”:”Mounting evidence suggests the answer is no.”,”summary”:”n
It's easy to blame running when a person who runs regularly develops arthritis. But that blame may be misguided. Here's a look at the latest research on the topic.
n “,”content”:”
nn  n
n
n
When I took up running in college, a friend of mine scoffed at the idea. He hated running and was convinced runners were “wearing out” their joints. He liked to say he was saving his knees for his old age.
n
So, was he onto something? Does running really ruin your joints, as many people believe?
n
Runners can get arthritis, but is running the cause?
n
You may think the answer is obvious. Surely, years of running (pounding pavements, or even softer surfaces) could wear out your joints, much like tires wear out after you put enough miles on them. And osteoarthritis, the most common type of arthritis, usually affects older adults. In fact, it’s often described as age-related and degenerative. That sounds like a wear-and-tear sort of situation, right?
n
Maybe not. Sure, it’s easy to blame running when a person who runs regularly develops arthritis. But that blame may be misguided. The questions to ask are:
n
- n
- Does running damage the joints and lead to arthritis?
- Does arthritis develop first and become more noticeable while running?
- Is the connection more complicated? Perhaps there’s no connection between running and arthritis for most people. But maybe those destined to develop arthritis (due to their genes, for example) get it sooner if they take up running.
n
n
n
n
Extensive research over the last several decades has investigated these questions. While the answers are still not entirely clear, we’re moving closer.
n
What is the relationship between running and arthritis?
n
Mounting evidence suggests that that running does not cause osteoarthritis, or any other joint disease.
n
- n
- A study published in 2017 found that recreational runners had lower rates of hip and knee osteoarthritis (3.5%) compared with competitive runners (13.3%) and nonrunners (10.2%).
- According to a 2018 study, the rate of hip or knee arthritis among 675 marathon runners was half the rate expected within the US population.
- A 2022 analysis of 24 studies found no evidence of significant harm to the cartilage lining the knee joints on MRIs taken just after running.
n
n
n
n
These are just a few of the published medical studies on the subject. Overall, research suggests that running is an unlikely cause of arthritis — and might even be protective.
n
Why is it hard to study running and arthritis?
n
- n
- Osteoarthritis takes many years to develop. Convincing research would require a long time, perhaps a decade or more.
- It’s impossible to perform an ideal study. The most powerful type of research study is a double-blind, randomized, controlled trial. Participants in these studies are assigned to a treatment group (perhaps taking a new drug) or a control group (often taking a placebo). Double-blind means neither researchers nor participants know which people are in the treatment group and which people are getting a placebo. When the treatment being studied is running, there’s no way to conduct this kind of trial.
- Beware the confounders. A confounder is a factor or variable you can’t account for in a study. There may be important differences between people who run and those who don’t that have nothing to do with running. For example, runners may follow a healthier diet, maintain a healthier weight, or smoke less than nonrunners. They may differ with respect to how their joints are aligned, the strength of their ligaments, or genes that direct development of the musculoskeletal system. These factors could affect the risk of arthritis and make study results hard to interpret clearly. In fact, they may explain why some studies find that running is protective.
- The effect of running may vary between people. For example, it’s possible, though not proven, that people with obesity who run regularly are at increased risk of arthritis due to the stress of excess weight on the joints.
n
n
n
n
n
The bottom line
n
Trends in recent research suggest that running does not wear out your joints. That should be reassuring for those of us who enjoy running. And if you don’t like to run, that’s fine: try to find forms of exercise that you enjoy more. Just don’t base your decision — or excuse — for not running on the idea that it will ruin your joints.
n “,”excerpt”:”n
It's easy to blame running when a person who runs regularly develops arthritis. But that blame may be misguided. Here's a look at the latest research on the topic.
n “,”short_excerpt”:”n
It's easy to blame running when a person who runs regularly develops arthritis. But that blame may be misguided. Here's a look at the latest research on the topic.
n “,”description”:null,”author”:null,”slug”:”does-running-cause-arthritis-202304262930″,”sort_date”:”2023-04-26T04:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2930,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL042623″,”publication_date”:”2023-04-26T14:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-05-05T14:17:57.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-05-01T04:00:00.000000Z”,”active”:1,”created_at”:”2023-04-26T09:00:02.000000Z”,”updated_at”:”2023-05-05T14:17:57.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:10,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:23,”cr_id”:2,”featured”:1,”hhp_staff”:1,”hidden”:0,”name”:”Robert H. Shmerling, MD”,”title”:null,”first_name”:”Robert”,”middle_name”:”H.”,”last_name”:”Shmerling”,”suffix”:”MD”,”slug”:”robert-h-shmerling-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing”,”description”:”
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. As a practicing rheumatologist for over 30 years, Dr. Shmerling engaged in a mix of patient care, teaching, and research. His research interests center on diagnostic studies in patients with musculoskeletal symptoms, and rheumatic and autoimmune diseases. He has published research regarding infectious arthritis, medical ethics, and diagnostic test performance in rheumatic disease. Having retired from patient care in 2019, Dr. Shmerling now works as a senior faculty editor for Harvard Health Publishing.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/OdKCKaVzyx3xPsUxIBc9zJz8m3zvysnJa3UJsGOd.jpg”,”twitter_username”:”RobShmerling”,”sort_order”:4,”created_at”:”2021-05-11T10:05:10.000000Z”,”updated_at”:”2023-09-06T15:33:18.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18039,”author_id”:23,”sort_order”:1}}],”contentable”:{“id”:2930,”comments_open”:1,”created_at”:”2023-04-26T09:00:02.000000Z”,”updated_at”:”2023-04-28T02:33:12.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:13852,”model_type”:”AppModelsMarketingContent”,”model_id”:18039,”uuid”:”050facb4-31f0-4bc5-a423-53be3c108afd”,”collection_name”:”contents”,”name”:”2434e7c0-3082-4e6a-9556-3e36e6f38b4c”,”file_name”:”2434e7c0-3082-4e6a-9556-3e36e6f38b4c.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:63937,”manipulations”:[],”custom_properties”:{“alt”:”A middle-aged man wearing a blue zip top and lighter blue track pants running alongside a blurred cityscape”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:13810,”created_at”:”2023-04-26T09:00:02.000000Z”,”updated_at”:”2023-04-26T09:00:10.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/13852/2434e7c0-3082-4e6a-9556-3e36e6f38b4c.jpg”}],”primary_content_topic”:{“id”:10,”name”:”Exercise & Fitness”,”slug”:”exercise-and-fitness”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/exercise-and-fitness”}},{“id”:18415,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Long-lasting C. diff infections: A threat to the gut”,”short_title”:””,”subheading”:”Severe diarrhea and colon inflammation can persist for months — or years — after infection occurs due to gut microbiome imbalances.”,”summary”:”n
Virtually everyone carries the bacteria Clostridioides difficile, or C. diff. But half a million Americans a year develop a serious C. diff infection due to a gut microbiome imbalance. It disproportionately strikes people in hospitals and nursing homes, and can recur repeatedly.
n “,”content”:”
n  n
n
n
If you’ve ever dealt with diarrhea, you know how quickly it leaves you feeling depleted. Now imagine a case that rages on and on — or comes back again and again.
n
This is the reality for nearly 500,000 Americans each year who have the bacterial infection known as Clostridioides difficile, or C. diff. Virulent diarrhea and inflammation of the colon can even turn life-threatening.
n
This primer will help you understand how C. diff spreads and releases toxins, what the common symptoms are, and who is most vulnerable. Dr. Jessica Allegretti, director of the fecal microbiota program at Harvard-affiliated Brigham and Women’s Hospital, also touches on promising preventive strategies and treatments.
n
How does C. diff spread?
n
Like many bacteria, C. diff is present in our stool. It’s carried by virtually everyone — on our skin and even on the soles of our shoes. When C. diff bacteria are outside the body, they are inactive spores. They only have a chance to become active when they’re swallowed and reach the intestines.
n
Even then, many people who swallow C. diff spores never become ill. The spores only sicken people whose gut microbiome — the trillions of organisms living in their intestines — becomes imbalanced for one of the various reasons described below. When an imbalance occurs, the spores start to multiply and create toxins that lead to a C. diff infection.
n
“Many of us are colonized with C. diff bacteria without any consequences,” says Dr. Allegretti. “We’re swallowing C. diff spores all the time. Only under the right circumstances will the spores germinate and release a toxin. It’s the toxin that makes you sick.”
n
What are the symptoms of a C. diff infection?
n
The symptoms mimic those of many other types of gastrointestinal ailments. Initially, this may make it difficult to tell the infection apart from milder illnesses.
n
Symptoms to watch for include
n
- n
- persistent diarrhea lasting three or more days
- nausea
- fever
- stomach pain or tenderness
- appetite loss.
n
n
n
n
n
n
“C. diff isn’t something that people in the general population should be walking around scared of,” Dr. Allegretti says. “But if you need to take an antibiotic, be on the lookout for diarrheal symptoms after finishing the course of antibiotics. Diarrhea that’s associated with antibiotics alone should resolve once you finish taking the medication.”
n
Who is most vulnerable?
n
A few sobering facts from the Centers for Disease Control (CDC):
n
- n
- C. diff is the top cause of health care-associated infections in the US.
- It disproportionately strikes people in hospitals and nursing homes.
- Among people over 65, one in 11 of those diagnosed with a health care-associated case of C. diff dies within a month.
n
n
n
n
However, other groups are also susceptible to the infection. Health care-associated C. diff infections are plateauing, Dr. Allegretti notes, while so-called community-based infections that occur among the general population are increasing.
n
People most likely to experience such infections:
n
- n
- Are taking antibiotics or have just finished a course of antibiotic therapy. People are up to 10 times more likely to get C. diff while on antibiotics or during the month afterward, according to the CDC. “Not everyone who takes an antibiotic gets C. diff, and not everyone who gets C. diff gets recurrent C. diff,” says Dr. Allegretti. “It has a lot to do with your host response, your gut microbiome, and your individual risk factors, such as immunosuppression or inflammatory bowel disease.”
- Have a weakened immune system due to cancer, organ transplant, or treatment with immunosuppressive drugs (such as people with inflammatory bowel disease or autoimmune conditions).
- Have close contact with someone who has been diagnosed with C. diff.
n
n
n
n
What prevention strategies help block the spread of C. diff?
n
Hospitals try to prevent C diff. among patients in several ways. They impose scrupulous hand-washing requirements among staff members. Patients who develop new diarrhea are tested for C. diff infection. Those who have it are isolated in their own rooms to help prevent further spread.
n
Outside of a hospital, you can help prevent this gut infection through a few commonsense measures.
n
- n
- Wash your hands thoroughly with soap and water every time you use the bathroom and always before eating. Clean hands are especially important if you’ve had C. diff or know you’ve been exposed to someone with it. By the way, alcohol-based hand sanitizer isn’t effective against C. diff because its organisms can form resistant spores.
- Take antibiotics only when strictly necessary and for the shortest period possible. “The biggest thing we can do is advocate for ourselves,” Dr. Allegretti says. “During cold and flu season, we know a lot of unnecessary antibiotic prescriptions are written for infections that are most likely viral, not bacterial. Antibiotics do not kill viruses — and unnecessary antibiotics may upset the bacterial balance in your gut. Ask your doctor: Do I need this prescription? Is there an alternative?”
- When you do need antibiotics, ask if a narrow-spectrum antibiotic would be effective for your type of infection. Why? Broad-spectrum antibiotics kill a wider array of bacteria. This may be overkill, depleting your gut microbiome unnecessarily and enabling C. diff bacteria to germinate. “The caveat is, we don’t want patients to not take antibiotics they need for an actual infection,” she says. “But have a conversation with your health care team.”
n
n
n
n
The type of antibiotic prescribed also matters, according to a 2023 study in the journal Open Forum Infectious Diseases. Researchers compared more than 159,000 people who had C. diff infection with 797,000 healthy controls. Study findings suggest that using clindamycin and later-generation cephalosporin antibiotics pose the greatest risk for C. diff infection. Meanwhile, the antibiotics minocycline and doxycycline were associated with the lowest risk.
n
“But there are very few safe antibiotics with regard to C. diff risk,” Dr. Allegretti says.
n
Can probiotics help prevent or treat C. diff infection?
n
Probiotics are live microorganisms that can help keep the gut healthy and are found in supplements, yogurt, and other fermented foods. Two familiar examples are various strains of Lactobacillus and Bifidobacterium.
n
However, probiotics haven’t been found to prevent C. diff or its recurrence. Research performed in mice and humans suggests that giving probiotics after a course of antibiotics may slow the pace of microbiome recovery. “You’re potentially delaying the recovery of your microbiome with probiotics,” she says.
n
How is C. diff infection treated?
n
Ironically, C. diff therapy typically starts with antibiotics, despite the infection’s proliferation due to antibiotic use. The antibiotics of choice include fidaxomicin or oral vancomycin.
n
However, about one in five people will suffer one or more recurrences –– and with each one, yet another recurrence becomes far likelier, Dr. Allegretti says. A repeat episode may happen because people haven’t disinfected their homes effectively. That leaves them open to reinfection with the same strain of C. diff while still vulnerable.
n
When C. diff recurs, fecal microbial transplants (FMT) are considered the gold standard treatment. FMT transplants fecal matter from a healthy donor into a patient’s gut, placing it there using an endoscope, enema, or within an oral capsule. This year, the FDA approved two live fecal microbiota products aimed at preventing recurrent C. diff infections.
n
“We haven’t gotten away from antibiotics yet to treat this disease,” says Dr. Allegretti. “But we have a lot of preventative strategies now. It’s certainly very exciting for people struggling with C. diff infections.”
“,”excerpt”:”n
Virtually everyone carries the bacteria Clostridioides difficile, or C. diff. But half a million Americans a year develop a serious C. diff infection due to a gut microbiome imbalance. It disproportionately strikes people in hospitals and nursing homes, and can recur repeatedly.
n “,”short_excerpt”:”n
Virtually everyone carries the bacteria Clostridioides difficile, or C. diff. But half a million Americans a year develop a serious C. diff infection due to a gut microbiome imbalance. It disproportionately strikes people in hospitals and nursing homes, and can recur repeatedly.
n “,”description”:null,”author”:null,”slug”:”long-lasting-c-diff-infections-a-threat-to-the-gut-202311012987″,”sort_date”:”2023-11-01T04:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2987,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL110123″,”publication_date”:”2023-11-01T14:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-01T09:00:03.000000Z”,”last_import_type”:”insert”,”last_modified_date”:”2023-10-31T04:00:00.000000Z”,”active”:1,”created_at”:”2023-11-01T09:00:03.000000Z”,”updated_at”:”2023-11-01T09:00:04.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:28,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:420,”cr_id”:779,”featured”:0,”hhp_staff”:0,”hidden”:0,”name”:”Maureen Salamon”,”title”:null,”first_name”:”Maureen”,”middle_name”:null,”last_name”:”Salamon”,”suffix”:null,”slug”:”maureen-salamon”,”byline”:”Executive Editor, Harvard Women's Health Watch“,”description”:”
Maureen Salamon is executive editor of Harvard Women’s Health Watch. She began her career as a newspaper reporter and later covered health and medicine for a wide variety of websites, magazines, and hospitals. Her work has appeared in The New York Times, The Atlantic, CNN.com, WebMD, Medscape and HealthDay, among other major outlets. Maureen earned a BA in print journalism from Penn State University.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/MWQyHwiFAPooqhDKsjTfFjCCCoIooqQNLj1M7LRO.jpg”,”twitter_username”:null,”sort_order”:0,”created_at”:”2022-02-24T21:39:38.000000Z”,”updated_at”:”2022-07-17T15:04:53.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18415,”author_id”:420,”sort_order”:1}}],”contentable”:{“id”:2987,”comments_open”:1,”created_at”:”2023-11-01T09:00:03.000000Z”,”updated_at”:”2023-11-01T09:00:03.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14485,”model_type”:”AppModelsMarketingContent”,”model_id”:18415,”uuid”:”1b736cad-d2cc-4242-874e-bf8e2ef87c34″,”collection_name”:”contents”,”name”:”39724b9a-bb07-43dc-9f0d-ad6badb52175″,”file_name”:”39724b9a-bb07-43dc-9f0d-ad6badb52175.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:100859,”manipulations”:[],”custom_properties”:{“alt”:”Gloved fingers holding lab dish with red scratches and dots of bacteria on clear growing media; concept is testing for C. diff “},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14431,”created_at”:”2023-11-01T09:00:04.000000Z”,”updated_at”:”2023-11-01T09:00:05.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14485/39724b9a-bb07-43dc-9f0d-ad6badb52175.jpg”}],”primary_content_topic”:{“id”:28,”name”:”Diseases & Conditions”,”slug”:”diseases-and-conditions”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/diseases-and-conditions”}},{“id”:18413,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”How much sleep do you actually need?”,”short_title”:””,”subheading”:”Sleep quality counts as much as hours logged.”,”summary”:”n
Just how many hours of sleep are enough for you? The answer varies and it might be better to track sleep quality than focus on the number of hours you log each night.
n “,”content”:”
n  n
n
n
On average, how many hours do you sleep each night? For most healthy adults, guidelines suggest at least seven hours of slumber.
n
But these are general recommendations and not strict rules. “Some people need less than seven hours, while others might need more,” says Eric Zhou with the Division of Sleep Medicine at Harvard Medical School.
n
Do you need more or less sleep time?
n
We get it: you know people who swear they only need five hours of sleep per night, yet you feel foggy unless you log in eight to nine hours. The major reason for individual differences is that we often look at sleep the wrong way.
n
“Instead of focusing exclusively on the number of hours we sleep per night, we should also consider our sleep quality,” says Zhou.
n
Sleep quality means how well you sleep during the night. Did you sleep straight through? Or did you have periods where you woke up? If so, did it take you a long time to fall asleep? How did you feel when you woke up?
n
“If you awaken refreshed and feel like you have the energy to get through your day, then I would worry less about the exact number of hours you’re sleeping,” says Zhou.
n
How does sleep quality affect your health?
n
Sleep quality is vital for our overall health. Research has shown that people with poor sleep quality are at a higher risk for diabetes, heart disease, stroke, and mental health issues like anxiety and depression.
n
And that’s not all. “Poor sleep also can increase daytime fatigue and make it more difficult to enjoy life,” says Zhou.
n
Yet it’s normal for people’s sleep patterns to change over time. “Many people are not going to sleep in their 50s and 60s exactly like they did in their 20s,” says Zhou.
n
Many of these changes are age-related. For instance, your circadian rhythm — which regulates many bodily functions, including our sleep-wake cycle — can naturally get disrupted over time. This means people spend less time each night in restorative slow-wave sleep.
n
Production of melatonin, the sleep hormone, also gradually declines with age. “As a result of these changes, when we get older we may start to wake up earlier than we did when we were younger, or wake up more frequently during the night,” says Zhou.
n
How can you track sleep quality?
n
How can you better understand the factors likely contributing to your sleep quality? One way is to keep a sleep diary where you track and record your sleep.
n
Every day, record the time you went to bed, how long it took you to fall asleep, whether you had any nighttime awakenings (and if so, how long you were awake), and at what time you woke up. Also, keep track of how you feel upon awakening and at the end of the day.
n
“After a week or two, review the information to see if you can identify certain patterns that may be affecting your sleep quality, then make adjustments,” says Zhou.
n
For example, if you have trouble falling asleep, go to bed half an hour later than usual but maintain the same wake-up time. “It is common for people struggling with their sleep to try to get more sleep by staying in bed longer, but this disrupts their sleep patterns and diminishes their sleep quality,” says Zhou.
n
Three key strategies to support the quality of your sleep
n
Other strategies that can help support good sleep quality include:
n
- n
- maintaining a consistent wake time, especially on weekends
- limiting daytime naps to 20 to 30 minutes, and at least six hours before the desired bedtime
- being physically active.
n
n
n
n
When it comes to sleep quality, consistency is vital. “People with good sleep quality often have a predictable sleep window where their sleep occurs,” says Zhou. “Good sleepers are likely to sleep around the same number of hours and stay asleep through the night.”
n
The bottom line on getting restful sleep
n
It’s unrealistic to expect perfect sleep every night. “If you have trouble sleeping one or two nights during the week, that can be related to the natural ebbs and flows of life,” says Zhou. “You may have eaten a big meal that day, drank too much alcohol while watching football, or had a stressful argument with someone. When tracking sleep quality, look at your overall sleep health week-to-week, not how you slept this Tuesday compared to last Tuesday.”
n
If you are doing all the right things for your sleep but still do not feel rested upon waking, talk to your doctor. This can help you rule out a sleep disorder like sleep apnea, or another health issue that can interfere with sleep such as acid reflux or high blood pressure. Other factors that can affect the quality of your sleep include taking multiple medicines, depression, anxiety, loneliness, and environmental changes like temperature, noise, and light exposure.
“,”excerpt”:”n
Just how many hours of sleep are enough for you? The answer varies and it might be better to track sleep quality than focus on the number of hours you log each night.
n “,”short_excerpt”:”n
Just how many hours of sleep are enough for you? The answer varies and it might be better to track sleep quality than focus on the number of hours you log each night.
n “,”description”:null,”author”:null,”slug”:”how-much-sleep-do-you-actually-need-202310302986″,”sort_date”:”2023-10-30T04:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2986,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL103023″,”publication_date”:”2023-10-30T14:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-10-27T09:00:03.000000Z”,”last_import_type”:”insert”,”last_modified_date”:”2023-10-26T04:00:00.000000Z”,”active”:1,”created_at”:”2023-10-27T09:00:03.000000Z”,”updated_at”:”2023-10-27T09:00:03.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:44,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:66,”cr_id”:434,”featured”:1,”hhp_staff”:0,”hidden”:0,”name”:”Matthew Solan”,”title”:null,”first_name”:”Matthew”,”middle_name”:null,”last_name”:”Solan”,”suffix”:null,”slug”:”matthew-solan”,”byline”:”Executive Editor, Harvard Men's Health Watch“,”description”:”
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s Women Nutrition Connection and Women’s Health Advisor. Matthew’s articles on medicine, exercise science, and nutrition have appeared in Men’s Health, Men’s Fitness, Muscle & Fitness, Runner’s World, and Yoga Journal. He earned a master of fine arts in writing from the University of San Francisco and a bachelor of science in journalism from the University of Florida.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/meFkQGpweKNzK8THXHlIORQI3ZZ68ShyfSRQykZN.jpg”,”twitter_username”:null,”sort_order”:0,”created_at”:”2021-05-11T10:26:17.000000Z”,”updated_at”:”2022-08-03T16:49:53.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18413,”author_id”:66,”sort_order”:1}}],”contentable”:{“id”:2986,”comments_open”:1,”created_at”:”2023-10-27T09:00:03.000000Z”,”updated_at”:”2023-10-27T09:00:03.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14476,”model_type”:”AppModelsMarketingContent”,”model_id”:18413,”uuid”:”a1e8eaa0-2138-44a4-ada3-5ac5a54be159″,”collection_name”:”contents”,”name”:”266d658e-36d0-4ae5-b500-b20c187947cc”,”file_name”:”266d658e-36d0-4ae5-b500-b20c187947cc.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:47004,”manipulations”:[],”custom_properties”:{“alt”:”Happy white and black-faced sheep clustered around a big gray alarm clock; crescent moon and clouds against lilac background, concept sleep”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14422,”created_at”:”2023-10-27T09:00:03.000000Z”,”updated_at”:”2023-10-27T09:00:06.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14476/266d658e-36d0-4ae5-b500-b20c187947cc.jpg”}],”primary_content_topic”:{“id”:44,”name”:”Staying Healthy”,”slug”:”staying-healthy”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/staying-healthy”}},{“id”:18040,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Lead poisoning: What parents should know and do”,”short_title”:””,”subheading”:”Reports of defective tests put lead poisoning — and ways to prevent it — back in the spotlight.”,”summary”:”n
Lead poisoning is a serious health risk for children. And yet, they may be exposed to lead in their daily lives. Learn the dangers of lead exposure and what you can do to keep your child safe.
n “,”content”:”
nn  n
n
n
You may have heard recent news reports about a company that knowingly sold defective lead testing machines that tested tens of thousands of children between 2013 and 2017. Or wondered about lead in tap water after the widely reported problems with lead-contaminated water in Flint, Michigan. Reports like these are reminders that parents need to be aware of lead — and do everything they can to keep their children safe.
n
How is lead a danger to health?
n
Lead is poisonous to the brain and nervous system, even in small amounts. There really is no safe level of lead in the blood. We particularly worry about children under the age of 6. Not only are their brains actively developing, but young children commonly touch lots of things — and put their hands in their mouths. Children who are exposed to lead can have problems with learning, understanding, and behavior that may be permanent.
n
How do children get exposed to lead?
n
In the US, lead used to be far more ubiquitous than it is now, particularly in paint and gas. Yet children can be exposed to lead in many ways.
n
- n
- Lead paint. In houses built before 1978, lead paint can sometimes be under other paint, and is most commonly found on windowsills or around doors. If there is peeling paint, children can sometimes ingest it. Dust from old paint can land on the floor or other surfaces that children touch with their hands (and then put their hands in their mouths). If there was ever lead paint on the outside of a house, it can sometimes be in the dirt around a house.
- Leaded gas. While leaded gas was outlawed in 1996, its use is still allowed in aircraft, farm equipment, racing cars, and marine engines.
- Water passing through lead pipes. Lead can be found in the water of older houses that have lead pipes.
- Other sources. Lead can also be found in some imported toys, candles, jewelry, and traditional medicines. Some parents may have exposure at work or through hobbies and bring it home on their hands or clothing. Examples include working in demolition of older houses, making things using lead solder, or having exposure to lead bullets at a firing range.
n
n
n
n
n
What can parents do to protect children from lead?
n
First, know about possible exposures.
n
- n
- If you have an older home, get it inspected for lead if you haven’t done so already. (If you rent, federal law requires landlords to disclose known lead-based paint hazards when you sign a lease.) Inspection is particularly important if you are planning renovations, which often create dust and debris that increase the risk of exposure. Your local health department can give you information about how to do this testing. If there is lead in your home, don’t try to remove it yourself! It needs to be done carefully, by a qualified professional, to be safe.
- Talk to your local health department about getting the water in your house tested. Even if your house is new, there can sometimes be older pipes in the water system. Using a water filter and taking other steps can reduce or eliminate lead in tap water.
- If you have an older home and live in an urban area, there can be lead in the soil. You may want to have the soil around your house tested for lead. Don’t let your child play in bare soil, and be sure they take off their shoes before coming in the house and wash their hands after being outside.
- Learn about lead in foods, cosmetics, and traditional medications.
- Learn about lead in toys, jewelry, and plastics (yet another reason to limit your child’s exposure to plastic).
n
n
n
n
n
n
Second, talk to your pediatrician about whether your child should have a blood test to check for lead poisoning. The American Academy of Pediatrics recommends:
n
- n
- Assessing young children for risk of exposure at all checkups between 6 months and 6 years of age, and
- Testing children if a risk is identified, particularly at 12 and 24 months. Living in an old home, or in a community with lots of older homes, counts as a risk. Given that low levels of lead exposure that can lead to lifelong problems do not cause symptoms, it’s always better to be safe than sorry. If there is any chance that your child might have an exposure, get them tested.
n
n
n
How is childhood lead exposure treated?
n
If your child is found to have lead in their blood, the most important next step is to figure out the exposure — and get rid of it. Once the child is no longer exposed, the lead level will go down, although it does so slowly.
n
Iron deficiency makes the body more vulnerable to lead poisoning. If your child has an iron deficiency it should be treated, but usually medications aren’t used unless lead levels are very high. In those cases, special medications called chelators are used to help pull the lead out of the blood.
n
For more information, visit the Centers for Disease Control and Prevention website on lead poisoning prevention.
n “,”excerpt”:”n
Lead poisoning is a serious health risk for children. And yet, they may be exposed to lead in their daily lives. Learn the dangers of lead exposure and what you can do to keep your child safe.
n “,”short_excerpt”:”n
Lead poisoning is a serious health risk for children. And yet, they may be exposed to lead in their daily lives. Learn the dangers of lead exposure and what you can do to keep your child safe.
n “,”description”:null,”author”:null,”slug”:”lead-poisoning-what-parents-should-know-and-do-202305012931″,”sort_date”:”2023-05-01T04:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2931,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL050123″,”publication_date”:”2023-05-01T14:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-05-09T09:00:03.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-05-08T04:00:00.000000Z”,”active”:1,”created_at”:”2023-04-29T09:00:02.000000Z”,”updated_at”:”2023-05-09T09:00:03.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:24,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:46,”cr_id”:4,”featured”:0,”hhp_staff”:1,”hidden”:0,”name”:”Claire McCarthy, MD”,”title”:null,”first_name”:”Claire”,”middle_name”:null,”last_name”:”McCarthy”,”suffix”:”MD”,”slug”:”claire-mccarthy-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing”,”description”:”Claire McCarthy, MD, is a primary care pediatrician at Boston Children’s Hospital, and an assistant professor of pediatrics at Harvard Medical School. In addition to being a senior faculty editor for Harvard Health Publishing, Dr. McCarthy writes about health and parenting for Boston Children’s Hospital, Boston.com, and the Huffington Post.”,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/mvCBqecmOmDXOhy74hH3DviJmMAprZqhFgGbhTJL.jpg”,”twitter_username”:null,”sort_order”:5,”created_at”:”2021-05-11T10:23:17.000000Z”,”updated_at”:”2023-09-05T22:36:44.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18040,”author_id”:46,”sort_order”:1}}],”contentable”:{“id”:2931,”comments_open”:1,”created_at”:”2023-04-29T09:00:02.000000Z”,”updated_at”:”2023-05-08T14:21:21.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:13853,”model_type”:”AppModelsMarketingContent”,”model_id”:18040,”uuid”:”746bd38a-930c-4882-8db8-61a9484b18c3″,”collection_name”:”contents”,”name”:”ffbadef4-72a7-4b93-9bb5-326d2c170b35″,”file_name”:”ffbadef4-72a7-4b93-9bb5-326d2c170b35.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:60618,”manipulations”:[],”custom_properties”:{“alt”:”Peeling pieces of paint arranged to spell the word lead; concept is lead poisoning”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:13811,”created_at”:”2023-04-29T09:00:02.000000Z”,”updated_at”:”2023-04-29T09:00:11.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/13853/ffbadef4-72a7-4b93-9bb5-326d2c170b35.jpg”}],”primary_content_topic”:{“id”:24,”name”:”Child & Teen Health”,”slug”:”child-and-teen-health”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/child-and-teen-health”}}], currentIndex: 0 }” x-on:slide-change.window=”currentIndex = $event.detail.currentIndex”>
Recent Blog Articles
Staying Healthy
The muscular organ that helps us speak, taste, and swallow has a certain look when it’s healthy.
By
Heidi Godman,
Executive Editor, Harvard Health Letter

If the eyes are the windows to the soul, then consider the tongue a sort of check-engine light for the body. The tongue’s appearance gives doctors an idea about certain aspects of your health, and its color is an important clue.
What should your tongue look like?
The tongue should have a rounded, symmetrical shape. It’s generally light pink, though it may have a little purple or brown pigmentation in African, Asian, and Mediterranean populations. It can also have a hint of white coating.
“The coating comes from a tough protein called keratin, which helps keep your tongue from being scratched when you eat,” says Dr. Tien Jiang, a prosthodontist in the Department of Oral Health Policy and Epidemiology at the Harvard School of Dental Medicine.
Up close, you might be able to see that your tongue is covered in tiny bumps (papillae) that serve several purposes:
- They sense temperature and touch.
- They contain taste buds that enable you to detect if food is sweet, salty, sour, bitter, or savory.
- They create friction to help you form a little ball of food (bolus) that you can swallow.
Can diet affect tongue color?
Yes. Sometimes diet may be partly to blame for a shift away from your usual tongue tone. That’s because the papillae can absorb the colors and residues of foods and drinks you consume. For example, that blue popsicle or candy you ate as a kid probably turned your tongue an exciting shade of azure. Coffee, tea, and many types of foods, such as curried dishes with lots of yellow turmeric, can also leave their marks.
Discoloration is usually just temporary, however. Drinking plenty of water and maintaining good oral hygiene will wash away food and dyes that cling to the tongue.
A dark or bright tongue, white patches, and other causes for concern
Some tongue colors and appearances are signs of health issues. Check with your doctor if you notice any of the following:
- A brown or black tongue signals a condition called “black hairy tongue.” This occurs when papillae get too long. These tiny bumps don’t usually get much chance to grow because they are shed regularly with all the activity in your mouth. If they do grow, they can trap bacteria and a mix of food colors, leading to the brown or black tinge. Risk factors include taking antibiotics or antihistamines, smoking, dry mouth, drinking excessive amounts of coffee or black tea, or poor oral hygiene.
- Thick white patches or white sores on the tongue probably mean you have an overgrowth of yeast in the mouth (thrush). Thrush can be triggered by conditions such as diabetes or HIV, side effects of antibiotics or cancer treatment, wearing dentures, smoking, dry mouth, or using steroid inhalers. In rare cases, white patches or sores are symptoms of oral cancer.
- If your tongue has painful red or yellow sores, you might be dealing with canker sores (irritated tissues), thrush (which can sometimes appear as red patches), or (in rare cases) oral cancer.
- A bright red tongue can indicate that you have a vitamin B12 deficiency or an infection called scarlet fever — a Streptococcus bacteria infection in the throat (strep throat) accompanied by a red body rash. If you have bright red patches that don’t hurt and seem to migrate from one place on the tongue to another, you might have a harmless, incurable condition called “geographic tongue.”
Should you brush your tongue or use a tongue scraper?
Good oral hygiene requires that you floss your teeth at least once a day and brush them at least twice a day. Take a few seconds to use the brush on your tongue.
“Stick out your tongue and swipe your toothbrush from the back of your tongue to the front: one swipe down the middle, one swipe down the left side, and one swipe down the right side. That helps remove bacteria and debris that collect in papillae,” Dr. Jiang says.
Some people swear by using a tongue scraper to clean the tongue. Dr. Jiang isn’t a fan, but doesn’t have a problem with someone using the tool, which is pulled forward on the tongue in a similar fashion to brushing the tongue. “The data about tongue scraper effectiveness are mixed,” she says. “It just comes down to what you’re willing to do daily to keep your tongue, teeth, mouth, and gums as healthy as possible.”
Worried about your tongue? What to do
If you’re worried about anything wrong with your tongue — especially if you also have a fever, a very sore throat, sores that won’t go away, or other new symptoms — call your primary care doctor or dentist.
Your doctor or dentist can
- assess your condition
- prescribe or suggest treatments to relieve discomfort, such as medicated mouthwashes or warm-water rinses
- urge you to stay hydrated and step up your oral hygiene.
If necessary, your doctor can refer you to a specialist for further evaluation.
About the Author

Heidi Godman,
Executive Editor, Harvard Health Letter
See Full Bio
About the Reviewer
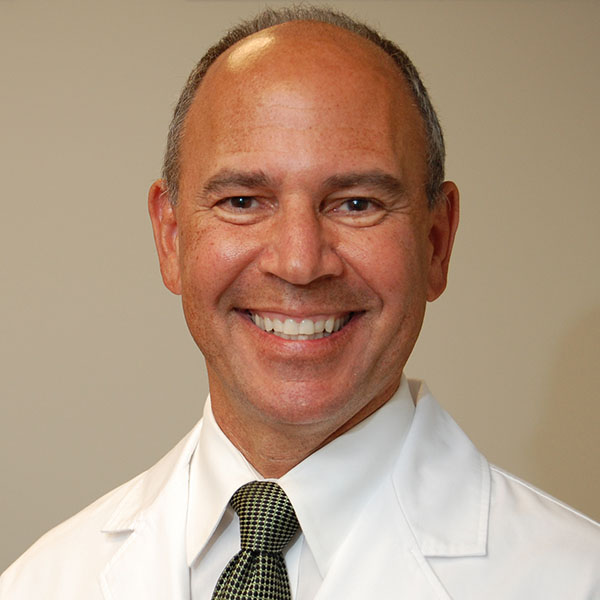
Howard E. LeWine, MD,
Chief Medical Editor, Harvard Health Publishing
See Full Bio
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
n  n
n
n
n Part 2 of a two-part series on making decisions about driving as we age. Read Part 1 here. n
n
It’s a simple but unfortunate fact: driving skills can wane over time.
n
Eventually, driving can become unsafe for an older driver, their passengers, and others on the road. If you notice a decline in driving abilities in a loved one, or in yourself, what’s the best way to handle this?
n
If you’re an older driver: Create an action plan
n
If you’re an older driver, don’t wait for a near-miss or an accident to think about the next steps. Planning ahead can help you tackle fixable issues, make necessary transitions easier, and avoid harming yourself or someone else.
n
Here are six measures you can take right now:
n
Have a frank conversation with a trusted friend or family member. After driving with them as a passenger, ask whether they are worried about your driving. Don’t disregard their comments, even if they share things you don’t want to hear.
n
See your doctor and talk about your driving. Is it harder to see at night? Are you finding you’re slower to react? Ask your doctor about medical care that can help, such as cataract surgery, treatment for sleep apnea, or adjustments to medications that might affect driving.
n
Take a self-evaluation test or an on-road test.AAA has tools to help with this, or you can check with your local department of motor vehicles for options. Even if you feel it’s unnecessary, a driving test can be reassuring to your loved ones that you’re still safe behind the wheel.
n
Take driving classes. In many places, there are general refresher courses, courses for defensive driving, and even simulators that don’t require actual road tests. AAA and AARP offer online courses that can help you improve your driving. (And by the way, these courses may also reduce the cost of your auto insurance!)
n
Consider alternatives to how you drive. Stick to roads that are close to home or to routes that have traffic lights (rather than having to decide when traffic is clear enough to turn). Consider giving up night driving if that is particularly difficult.
n
Make adjustments to your car that can help. Examples include using a steering wheel cover to improve your grip or changing the position of your seat to improve your view of the road. Check out the CarFit program that aims to optimize the “fit” of a driver in their car.
n
In addition, explore options that don’t require you to drive as often or at all:
n
- n
- grocery delivery
- public or senior transportation (if offered or available where you live)
- carpooling with friends or family
- ride-hailing services or taxis
- hiring a driver.
n
n
n
n
n
n
Cost and availability may be barriers, but it’s worth looking into these options.
n
If you’re a concerned family member or friend: Start a conversation
n
With so much at stake, the language you use matters. So, it’s a good idea to think ahead about how to talk about these challenges.
n
Put safety and solutions first. It’s best not to lead by criticizing driving skills. Instead, talk about driving with safety and solutions in mind, such as the options described above.
n
Choose your words carefully. It helps to avoid threats or confrontational language: rather than saying “Your driving is terrible so I’ve taken away your keys,” focus on safety and support:
n
- n
- n
- n
- n Let’s talk about how I can help so you don’t have to drive. I can drive you to get your groceries on Sundays and we can make a day of it!n
- n How do you think those dents got on your car? Are you having trouble with your vision?n
- We’d all feel terrible if you had an accident and got hurt or hurt someone else.
n
n
n
n
n
n
Offer to go for a ride together and then to talk about specific concerns, such as staying in the proper lane, changing lanes, making left-hand turns, speed, or sudden braking. Encourage consideration of a self-evaluation or on-road test, and driving classes to help polish skills.
n
Use examples from familiar experiences. It can be helpful to remind your loved one how his or her parents or grandparents had to cut back on their driving, or how an older neighbor was an unsafe driver.
n
Focus on the risks posed by other drivers. Aggressive or unpredictable drivers can pose more danger to older drivers with slower reaction times.
n
How else can families or friends of older drivers be helpful?
n
- n
- Consider whether to contact their doctor. Ask their doctor if it’s possible to talk with your loved one or friend about their driving. State regulations vary on mandatory reporting of conditions that affect a patient’s ability to drive. Be aware that some doctors may be reluctant to report their patients to their registry of motor vehicles, due to concerns about patient privacy or jeopardizing the patient-doctor relationship.
- Look into rules and regulations around older drivers where your loved one lives. Illinois is currently the only state that requires a road test for older drivers. But many states require vision tests and in-person renewal with increasing frequency for older drivers.
- Consider reporting an unsafe driver to traffic safety authorities. This may feel like a betrayal, but if other efforts have failed this option might be better than waiting until there’s a serious accident.
n
n
n
n
The bottom line
n
In the future, safe, driverless cars may be a solution to the challenge of waning driving skills among older drivers. But we’re not there yet.
n
Right now, we should all acknowledge that it’s not easy to address concerns about impaired older drivers. My best advice is that older drivers and their loved ones try to talk about ways to remain a safe driver and put a plan in place. Ideally, we all would start the conversation well before any driving problems are evident.
n
And it may take more than one conversation. Many more. But let’s face it: sooner or later, most drivers will have to stop driving. For some older drivers, that time may be now. For the rest of us, recognizing this eventuality could help when our time comes.
n “,”excerpt”:”n
Many people experience a decline in their driving skills as they age. While some choose to stop driving, others resist. Whether it’s you or a loved one, planning ahead can help you tackle fixable issues, make transitions easier, and avoid harming yourself or someone else.
n “,”short_excerpt”:”n
Many people experience a decline in their driving skills as they age. While some choose to stop driving, others resist. Whether it’s you or a loved one, planning ahead can help you tackle fixable issues, make transitions easier, and avoid harming yourself or someone else.
n “,”description”:null,”author”:null,”slug”:”what-to-do-when-driving-skills-decline-202311152991″,”sort_date”:”2023-11-15T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2991,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL111523″,”publication_date”:”2023-11-15T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-16T10:00:04.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-11-15T05:00:00.000000Z”,”active”:1,”created_at”:”2023-11-15T10:00:03.000000Z”,”updated_at”:”2023-11-16T10:00:04.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:44,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:23,”cr_id”:2,”featured”:1,”hhp_staff”:1,”hidden”:0,”name”:”Robert H. Shmerling, MD”,”title”:null,”first_name”:”Robert”,”middle_name”:”H.”,”last_name”:”Shmerling”,”suffix”:”MD”,”slug”:”robert-h-shmerling-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing”,”description”:”
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. As a practicing rheumatologist for over 30 years, Dr. Shmerling engaged in a mix of patient care, teaching, and research. His research interests center on diagnostic studies in patients with musculoskeletal symptoms, and rheumatic and autoimmune diseases. He has published research regarding infectious arthritis, medical ethics, and diagnostic test performance in rheumatic disease. Having retired from patient care in 2019, Dr. Shmerling now works as a senior faculty editor for Harvard Health Publishing.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/OdKCKaVzyx3xPsUxIBc9zJz8m3zvysnJa3UJsGOd.jpg”,”twitter_username”:”RobShmerling”,”sort_order”:4,”created_at”:”2021-05-11T10:05:10.000000Z”,”updated_at”:”2023-09-06T15:33:18.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18425,”author_id”:23,”sort_order”:1}}],”contentable”:{“id”:2991,”comments_open”:1,”created_at”:”2023-11-15T10:00:03.000000Z”,”updated_at”:”2023-11-15T10:00:03.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14502,”model_type”:”AppModelsMarketingContent”,”model_id”:18425,”uuid”:”3f091965-a498-4d6a-a299-8fdeeb9dfcfb”,”collection_name”:”contents”,”name”:”bcb42e0d-03e3-4752-8f23-2286f283fb97″,”file_name”:”bcb42e0d-03e3-4752-8f23-2286f283fb97.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:41089,”manipulations”:[],”custom_properties”:{“alt”:”A square-topped gold car key and a gold car on a key ring against a deep yellow background”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14448,”created_at”:”2023-11-15T10:00:03.000000Z”,”updated_at”:”2023-11-15T10:00:04.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14502/bcb42e0d-03e3-4752-8f23-2286f283fb97.jpg”}],”primary_content_topic”:{“id”:44,”name”:”Staying Healthy”,”slug”:”staying-healthy”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/staying-healthy”}},{“id”:18426,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”A tough question: When should an older driver stop driving?”,”short_title”:””,”subheading”:”Be alert to red flags suggesting that a family member — or you — should consider hanging up the keys.”,”summary”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”content”:”
nn  n
n
n
n Part 1 of a two-part series on making decisions about driving as we age. Read Part 2 here. n
n
When my grandmother repeatedly clipped the mailbox backing out of her driveway, she always had a ready explanation: “the sun was in my eyes” or “your grandfather distracted me.” Our family knew we needed to take action. But no one wanted to be the one to ask her to stop driving. She was fiercely independent, didn’t agree that her driving was a problem, and didn’t appreciate our concerns.
n
Maybe there’s a similar story unfolding in your family. Or maybe you’re starting to wonder about your own skills. As part one in a two-part series, this post aims to help people understand red flags to watch for, and why driving abilities change as people age. It also describes a few ways to improve impaired driving, and challenges to navigate.
n
A second post will address ways to strike a balance that respects dignity — and safety — while providing action plans for older drivers and their families.
n
How safe are older drivers on the road?
n
Unsafe drivers can be any age, particularly when drinking is involved. But fatal traffic accidents have risen in both young drivers and older drivers, according to data from the National Safety Council:
n
- n
- Fatalities occurring in crashes involving a driver ages 15 to 20 rose nearly 10% between 2020 and 2021, accounting for 5,565 deaths.
- Among drivers 65 or older, fatalities rose 15% between 2020 and 2021, accounting for more than 8,200 deaths.
n
n
n
While younger drivers may be inexperienced or more likely to be distracted or reckless, older drivers often overestimate their driving abilities. That may be one reason many unsafe older drivers continue to drive despite failing driving skills.
n
Per mile driven, the rate of motor vehicle accidents is higher for drivers ages 80 and older than for almost every other age group, according to the Insurance Institute for Highway Safety. Only the youngest drivers have higher rates. And the rate of fatal motor vehicle accidents per mile driven is higher for drivers aged 85 and older than for every other age group.
n
These statistics reflect the reality that an older driver may not be the only one injured or killed in a crash — occupants in one or more vehicles may be, too. And then there are pedestrians and cyclists at risk.
n
Clearly, the stakes are high when any unsafe driver is on the road. For older drivers with waning driving skills, it’s important to recognize the problem and understand why it’s happening. The following four steps are a good start.
n
1. Seeing any red flags?
n
As people get older, driving skills may decline so slowly that it’s not obvious worrisome changes are happening. Even when mishaps and near-misses occur, there are so many possible contributors —especially other drivers — that it may not be clear that the older driver was at fault.
n
Red flags that might mean an older person is an unsafe driver include:
n
- n
- concerned comments from family or friends
- reluctance of others to ride with them
- input from other drivers (why is everyone honking at me?) or traffic authorities (why am I getting all these traffic tickets?)
- getting lost on familiar roads
- consistently driving too slowly or too fast
- unexplained dents or scratches appearing on the car
- frequent accidents or near-misses.
n
n
n
n
n
n
n
n
2. Why do driving skills tend to wane with age?
n
While people of advanced age can safely drive (and many do!), driving skills may wane due to:
n
- n
- medical conditions, such as arthritis, neuropathy, or dementia
- medications, such as sedatives or certain antidepressants
- age-related changes in reaction time
- trouble with vision or hearing
- other physical changes related to aging, such as less flexibility or strength
- difficulty processing rapidly changing information. For example, an older driver may be more likely than a younger driver to accidentally press the gas pedal instead of the brake when needing to stop suddenly.
n
n
n
n
n
n
n
3. What can — and can’t — be reversed to improve driving?
n
Some changes that impair driving can be reversed or a workaround can be found. For example, if driving is impaired due to cataracts, cataract surgery can restore vision and improve driving. If night driving is difficult, it’s best to drive only during the day. If memory problems are starting to arise, it may still be possible to drive safely in more limited circumstances.
n
Driving problems due to advanced dementia or a major stroke affecting judgment and physical skills are much less likely to improve.
n
4. Accept that conversations about not driving are challenging
n
If there is no simple way to reverse or work around declining driving skills, accept that there will be many challenges to navigate, whether you’re the older driver or a family member.
n
Challenges facing the driver:
n
- n
- It’s not easy to acknowledge declining function. Driving impairment is an unsettling milestone, an indication that the future may include further loss of abilities.
- It can feel unnecessary and unreasonable. Most older folks facing a decision about whether it’s safe to continue driving were good drivers not so long ago. They may still see themselves as competent drivers, and see efforts to restrict their driving as overly cautious or demeaning.
- Denial and defensiveness are common. Even when all the signs are there, it may be tempting for a poor driver to deflect blame (for example, blaming other drivers).
- Not driving is a loss of independence. Sure, there are other ways to get around and nondrivers can certainly be independent. But few alternatives rival the independence that comes with being able to drive yourself. And, depending on where you live, public transportation or other alternatives to driving may be limited.
n
n
n
n
n
Challenges facing the family:
n
- n
- Often, the older driver doesn’t share their family’s concerns about driving safety. This can lead to arguments, confrontation, and resentment.
- The safety of others is at stake. The older driver with waning skills may endanger many people besides themselves: passengers in their care, other drivers and their passengers, cyclists, and pedestrians.
- It’s hard to know when the time is right. Speaking up too soon may lead to unnecessary restrictions on a loved one’s favored means of transportation, not to mention family strife. Waiting too long can lead to avoidable tragedy.
n
n
n
n
Finding a path forward
n
As for my grandmother, none of us knew what to say. Should we try to get her to agree to stop driving entirely or let her ease into the idea over time? Maybe she could stop driving at night or limit her driving to short distances. Should we bring it to the attention of her doctor and let them direct the next steps? Or should we take an even harder step and report her to the authorities?
n
If you’re asking similar questions — or if you’re starting to wonder about your own driving abilities — you may feel strongly that it’s important to respect individual preferences, dignity, and independence. Yet you also want to protect everyone from harm.
n
What are the best ways to strike a balance? Can you test and improve how an older driver is doing behind the wheel? Can you navigate tough conversations in ways that allow room for both independence and safety? These are the subjects to be tackled in Part 2.
n “,”excerpt”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”short_excerpt”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”description”:null,”author”:null,”slug”:”a-tough-question-when-should-an-older-driver-stop-driving-202311132992″,”sort_date”:”2023-11-13T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2992,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL111323″,”publication_date”:”2023-11-13T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-16T10:00:03.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-11-15T05:00:00.000000Z”,”active”:1,”created_at”:”2023-11-15T21:34:38.000000Z”,”updated_at”:”2023-11-16T10:00:03.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:44,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:23,”cr_id”:2,”featured”:1,”hhp_staff”:1,”hidden”:0,”name”:”Robert H. Shmerling, MD”,”title”:null,”first_name”:”Robert”,”middle_name”:”H.”,”last_name”:”Shmerling”,”suffix”:”MD”,”slug”:”robert-h-shmerling-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing”,”description”:”
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. As a practicing rheumatologist for over 30 years, Dr. Shmerling engaged in a mix of patient care, teaching, and research. His research interests center on diagnostic studies in patients with musculoskeletal symptoms, and rheumatic and autoimmune diseases. He has published research regarding infectious arthritis, medical ethics, and diagnostic test performance in rheumatic disease. Having retired from patient care in 2019, Dr. Shmerling now works as a senior faculty editor for Harvard Health Publishing.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/OdKCKaVzyx3xPsUxIBc9zJz8m3zvysnJa3UJsGOd.jpg”,”twitter_username”:”RobShmerling”,”sort_order”:4,”created_at”:”2021-05-11T10:05:10.000000Z”,”updated_at”:”2023-09-06T15:33:18.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18426,”author_id”:23,”sort_order”:1}}],”contentable”:{“id”:2992,”comments_open”:1,”created_at”:”2023-11-15T21:34:38.000000Z”,”updated_at”:”2023-11-15T21:34:38.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14503,”model_type”:”AppModelsMarketingContent”,”model_id”:18426,”uuid”:”253e11aa-2393-4c3c-af23-b812d32e9c0c”,”collection_name”:”contents”,”name”:”f6fd51a8-b6bf-4a40-9b61-0067cf611802″,”file_name”:”f6fd51a8-b6bf-4a40-9b61-0067cf611802.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:70537,”manipulations”:[],”custom_properties”:{“alt”:”Abstract of traffic on city highway at night with glaring headlights forming big, colored dots “},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14449,”created_at”:”2023-11-15T21:34:38.000000Z”,”updated_at”:”2023-11-15T21:34:41.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14503/f6fd51a8-b6bf-4a40-9b61-0067cf611802.jpg”}],”primary_content_topic”:{“id”:44,”name”:”Staying Healthy”,”slug”:”staying-healthy”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/staying-healthy”}},{“id”:18427,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”A tough question: When should an older driver stop driving?”,”short_title”:””,”subheading”:”Be alert to red flags suggesting that a family member – or you –– should consider hanging up the keys.”,”summary”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”content”:”
n  n
n
n
n Part 1 of a two-part series on making decisions about driving as we age. Read Part 2 here. n
n
When my grandmother repeatedly clipped the mailbox backing out of her driveway, she always had a ready explanation: “the sun was in my eyes” or “your grandfather distracted me.” Our family knew we needed to take action. But no one wanted to be the one to ask her to stop driving. She was fiercely independent, didn’t agree that her driving was a problem, and didn’t appreciate our concerns.
n
Maybe there’s a similar story unfolding in your family. Or maybe you’re starting to wonder about your own skills. As part one in a two-part series, this post aims to help people understand red flags to watch for, and why driving abilities change as people age. It also describes a few ways to improve impaired driving, and challenges to navigate.
n
A second post will address ways to strike a balance that respects dignity — and safety — while providing action plans for older drivers and their families.
n
How safe are older drivers on the road?
n
Unsafe drivers can be any age, particularly when drinking is involved. But fatal traffic accidents have risen in both young drivers and older drivers, according to data from the National Safety Council:
n
- n
- Fatalities occurring in crashes involving a driver ages 15 to 20 rose nearly 10% between 2020 and 2021, accounting for 5,565 deaths.
- Among drivers 65 or older, fatalities rose 15% between 2020 and 2021, accounting for more than 8,200 deaths.
n
n
n
While younger drivers may be inexperienced or more likely to be distracted or reckless, older drivers often overestimate their driving abilities. That may be one reason many unsafe older drivers continue to drive despite failing driving skills.
n
Per mile driven, the rate of motor vehicle accidents is higher for drivers ages 80 and older than for almost every other age group, according to the Insurance Institute for Highway Safety. Only the youngest drivers have higher rates. And the rate of fatal motor vehicle accidents per mile driven is higher for drivers aged 85 and older than for every other age group.
n
These statistics reflect the reality that an older driver may not be the only one injured or killed in a crash — occupants in one or more vehicles may be, too. And then there are pedestrians and cyclists at risk.
n
Clearly, the stakes are high when any unsafe driver is on the road. For older drivers with waning driving skills, it’s important to recognize the problem and understand why it’s happening. The following four steps are a good start.
n
1. Seeing any red flags?
n
As people get older, driving skills may decline so slowly that it’s not obvious worrisome changes are happening. Even when mishaps and near-misses occur, there are so many possible contributors —especially other drivers — that it may not be clear that the older driver was at fault.
n
Red flags that might mean an older person is an unsafe driver include:
n
- n
- concerned comments from family or friends
- reluctance of others to ride with them
- input from other drivers (why is everyone honking at me?) or traffic authorities (why am I getting all these traffic tickets?)
- getting lost on familiar roads
- consistently driving too slowly or too fast
- unexplained dents or scratches appearing on the car
- frequent accidents or near-misses.
n
n
n
n
n
n
n
n
2. Why do driving skills tend to wane with age?
n
While people of advanced age can safely drive (and many do!), driving skills may wane due to:
n
- n
- medical conditions, such as arthritis, neuropathy, or dementia
- medications, such as sedatives or certain antidepressants
- age-related changes in reaction time
- trouble with vision or hearing
- other physical changes related to aging, such as less flexibility or strength
- difficulty processing rapidly changing information. For example, an older driver may be more likely than a younger driver to accidentally press the gas pedal instead of the brake when needing to stop suddenly.
n
n
n
n
n
n
n
3. What can — and can’t — be reversed to improve driving?
n
Some changes that impair driving can be reversed or a workaround can be found. For example, if driving is impaired due to cataracts, cataract surgery can restore vision and improve driving. If night driving is difficult, it’s best to drive only during the day. If memory problems are starting to arise, it may still be possible to drive safely in more limited circumstances.
n
Driving problems due to advanced dementia or a major stroke affecting judgment and physical skills are much less likely to improve.
n
4. Accept that conversations about not driving are challenging
n
If there is no simple way to reverse or work around declining driving skills, accept that there will be many challenges to navigate, whether you’re the older driver or a family member.
n
Challenges facing the driver:
n
- n
- It’s not easy to acknowledge declining function. Driving impairment is an unsettling milestone, an indication that the future may include further loss of abilities.
- It can feel unnecessary and unreasonable. Most older folks facing a decision about whether it’s safe to continue driving were good drivers not so long ago. They may still see themselves as competent drivers, and see efforts to restrict their driving as overly cautious or demeaning.
- Denial and defensiveness are common. Even when all the signs are there, it may be tempting for a poor driver to deflect blame (for example, blaming other drivers).
- Not driving is a loss of independence. Sure, there are other ways to get around and nondrivers can certainly be independent. But few alternatives rival the independence that comes with being able to drive yourself. And, depending on where you live, public transportation or other alternatives to driving may be limited.
n
n
n
n
n
Challenges facing the family:
n
- n
- Often, the older driver doesn’t share their family’s concerns about driving safety. This can lead to arguments, confrontation, and resentment.
- The safety of others is at stake. The older driver with waning skills may endanger many people besides themselves: passengers in their care, other drivers and their passengers, cyclists, and pedestrians.
- It’s hard to know when the time is right. Speaking up too soon may lead to unnecessary restrictions on a loved one’s favored means of transportation, not to mention family strife. Waiting too long can lead to avoidable tragedy.
n
n
n
n
Finding a path forward
n
As for my grandmother, none of us knew what to say. Should we try to get her to agree to stop driving entirely or let her ease into the idea over time? Maybe she could stop driving at night or limit her driving to short distances. Should we bring it to the attention of her doctor and let them direct the next steps? Or should we take an even harder step and report her to the authorities?
n
If you’re asking similar questions — or if you’re starting to wonder about your own driving abilities — you may feel strongly that it’s important to respect individual preferences, dignity, and independence. Yet you also want to protect everyone from harm.
n
What are the best ways to strike a balance? Can you test and improve how an older driver is doing behind the wheel? Can you navigate tough conversations in ways that allow room for both independence and safety? These are the subjects to be tackled in Part 2.
“,”excerpt”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”short_excerpt”:”n
Navigating whether or when an older person should limit or stop driving is tricky. Whether these concerns are about a family member or yourself, it’s helpful to understand how driving abilities –– and risk for motor vehicle accidents –– change with age and know red flags to watch for.
n “,”description”:null,”author”:null,”slug”:”a-tough-question-when-should-an-older-driver-stop-driving-202311132993″,”sort_date”:”2023-11-13T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2993,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL11132023″,”publication_date”:”2023-11-13T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-16T10:00:05.000000Z”,”last_import_type”:”insert”,”last_modified_date”:”2023-11-15T05:00:00.000000Z”,”active”:1,”created_at”:”2023-11-16T10:00:05.000000Z”,”updated_at”:”2023-11-16T10:00:05.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:44,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:23,”cr_id”:2,”featured”:1,”hhp_staff”:1,”hidden”:0,”name”:”Robert H. Shmerling, MD”,”title”:null,”first_name”:”Robert”,”middle_name”:”H.”,”last_name”:”Shmerling”,”suffix”:”MD”,”slug”:”robert-h-shmerling-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing”,”description”:”
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. As a practicing rheumatologist for over 30 years, Dr. Shmerling engaged in a mix of patient care, teaching, and research. His research interests center on diagnostic studies in patients with musculoskeletal symptoms, and rheumatic and autoimmune diseases. He has published research regarding infectious arthritis, medical ethics, and diagnostic test performance in rheumatic disease. Having retired from patient care in 2019, Dr. Shmerling now works as a senior faculty editor for Harvard Health Publishing.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/OdKCKaVzyx3xPsUxIBc9zJz8m3zvysnJa3UJsGOd.jpg”,”twitter_username”:”RobShmerling”,”sort_order”:4,”created_at”:”2021-05-11T10:05:10.000000Z”,”updated_at”:”2023-09-06T15:33:18.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18427,”author_id”:23,”sort_order”:1}}],”contentable”:{“id”:2993,”comments_open”:1,”created_at”:”2023-11-16T10:00:05.000000Z”,”updated_at”:”2023-11-16T10:00:05.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14504,”model_type”:”AppModelsMarketingContent”,”model_id”:18427,”uuid”:”3b34d315-4952-4834-b625-2ad8ce40b497″,”collection_name”:”contents”,”name”:”f6fd51a8-b6bf-4a40-9b61-0067cf611802″,”file_name”:”f6fd51a8-b6bf-4a40-9b61-0067cf611802.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:70537,”manipulations”:[],”custom_properties”:{“alt”:”Abstract of traffic on city highway at night with glaring headlights forming big, colored dots “},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14450,”created_at”:”2023-11-16T10:00:05.000000Z”,”updated_at”:”2023-11-16T10:00:06.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14504/f6fd51a8-b6bf-4a40-9b61-0067cf611802.jpg”}],”primary_content_topic”:{“id”:44,”name”:”Staying Healthy”,”slug”:”staying-healthy”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/staying-healthy”}},{“id”:17918,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”3 ways to create community and counter loneliness”,”short_title”:””,”subheading”:”Breaking through loneliness to build connections and enhance well-being.”,”summary”:”n
Loneliness boosts risk for many health problems, and can even contribute to an early death. Many people find it hard to reach out to make new friends, but there are strategies that can help.
n “,”content”:”
nn  n
n
n
Loneliness is complicated. You can feel lonely when you lack friends and miss companionship, or when you’re surrounded by people — even friends and family.
n
Either way, loneliness can have devastating health effects. It boosts risk for coronary artery disease, stroke, depression, high blood pressure, declining thinking skills, inability to perform daily living tasks, and even an early death. The remedy? Below we offer three ways to ease loneliness and add happiness by helping you expand your social network.
n
Taking the first steps
n
Not all loneliness can be solved by seeking out people. Loneliness that occurs despite relationships may require talk therapy and a journey that looks inward.
n
Reducing loneliness caused by a lack of relationships is more of an outward journey to make new friends. “That’s a challenge as we get older, because people are often established in their social groups and aren’t as available as they might have been in a different phase of life. So you have to be more entrepreneurial and work harder to make friends than you once did,” says Dr. Jacqueline Olds, a psychiatrist at Harvard-affiliated McLean Hospital and the coauthor of two books on loneliness.
n
Trying these strategies can help.
n
1. Seek like-minded souls
n
Being around people who share your interests gives you a head start on making friends: you already have something in common.
n
Start by considering your interests. Are you a voracious reader, a history lover, a movie aficionado, a gardener, a foodie, a puppy parent, or an athlete? Are you passionate about a cause, your community, or your heritage? Do you collect things? Do you love classic cars? Do you enjoy sprucing up old furniture? Maybe you want to learn something new, like how to cook Chinese food or speak another language. Search for online groups, in-person clubs, volunteer opportunities, or classes that match any of your interests or things you’d like to try.
n
Once you join a group, you’ll need to take part in it regularly to build bonds. If you can gather in person, it’s even better. “The part of our brain involved in social connection is stimulated by all five senses. When you’re with someone in the same room, you get a much stronger set of stimuli than you do by watching them on an electronic screen,” Dr. Olds says.
n
2. Create opportunities
n
If joining someone else’s group is unappealing, start your own. Host gatherings at your place or elsewhere. “All it takes is three people. You can say, ‘Let’s read books or talk about a TV show or have a dinner group on a regular basis,'” Dr. Olds says.
n
Other ideas for gatherings — either weekly or monthly — include:
n
- n
- game nights
- trivia nights
- hikes in interesting parks
- beach walks
- bird-watching expeditions
- running or cycling
- n meditationn
- museum visits
- cooking
- knitting, sewing, or crafting
- shopping
- day trips to nearby towns
- jewelry making
- collector show-and-tell (comic books, antique dolls, baseball cards).
n
n
n
n
n
n
n
n
n
n
n
n
n
n
n
The people you invite don’t have to be dear friends; they can just be people you’d like to get to know better — perhaps neighbors or work acquaintances.
n
If they’re interested in a regular gathering, pin down dates and times. Otherwise, the idea might stay stuck in the talking stages. “Don’t be timid. Say, ‘Let’s get our calendars out and get this scheduled,'” Dr. Olds says.
n
3. Brush up your social skills
n
Sometimes we’re rusty in surface social graces that help build deeper connections. “It makes a huge difference when you can be enthusiastic rather than just sitting there and hoping someone will realize how interesting you are,” Dr. Olds says.
n
Tips to practice:
n
- n
- Smile more. Smiling is welcoming, inviting, and hospitable to others.
- Be engaging. Prepare a few topics to talk about or questions to ask — perhaps about the news or the reason you’ve gathered (if it’s a seminar, for example, ask how long someone has been interested in the subject). Or look for a conversation starter. “Maybe the person is wearing a pretty brooch. Ask if there’s a story behind it,” Dr. Olds suggests.
- Be a good listener. “Listen in a way that someone realizes you’re paying attention. Hold their gaze, nod your head or say ‘Mm hmm’ as they’re talking so you give feedback. Assume everyone in the world is just yearning for your feedback,” Dr. Olds says.
- Ask follow-up questions. Don’t ignore signals that someone has interesting stories to tell. “If they allude to something, your job is to look fascinated and ask if they can tell you more. They’re dropping crumbs on a path to a deeper exchange,” Dr. Olds notes.
n
n
n
n
n
Even chats that don’t lead to friendships can be enriching. A 2022 study found that people who had the most diverse portfolios of social interactions — exchanges with strangers, acquaintances, friends, or family members — were much happier than those with the least diverse social portfolios.
n
Ultimately, a wide variety of interactions contributes to well-being, whether you’re talking to the cashier at the supermarket, a neighbor, an old friend, or a new one. And all of these connections combined may go a long way toward helping you feel less lonely.
n “,”excerpt”:”n
Loneliness boosts risk for many health problems, and can even contribute to an early death. Many people find it hard to reach out to make new friends, but there are strategies that can help.
n “,”short_excerpt”:”n
Loneliness boosts risk for many health problems, and can even contribute to an early death. Many people find it hard to reach out to make new friends, but there are strategies that can help.
n “,”description”:null,”author”:null,”slug”:”3-ways-to-create-community-and-counter-loneliness-202303082900″,”sort_date”:”2023-03-08T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2900,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”Bl030823″,”publication_date”:”2023-03-08T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-04-23T09:00:13.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-04-22T04:00:00.000000Z”,”active”:1,”created_at”:”2023-03-08T10:00:02.000000Z”,”updated_at”:”2023-04-23T09:00:13.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:37,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:31,”cr_id”:117,”featured”:0,”hhp_staff”:0,”hidden”:0,”name”:”Heidi Godman”,”title”:null,”first_name”:”Heidi”,”middle_name”:null,”last_name”:”Godman”,”suffix”:null,”slug”:”heidi-godman”,”byline”:”Executive Editor, Harvard Health Letter“,”description”:”
Heidi Godman is the executive editor of the Harvard Health Letter. Before coming to the Health Letter, she was an award-winning television news anchor and medical reporter for 25 years. Heidi was named a journalism fellow of the American Academy of Neurology, and has been honored by the Associated Press, the American Heart Association, the Wellness Community, and other organizations for outstanding medical reporting. Heidi holds a bachelor of science degree in journalism from West Virginia University.
“,”image_url”:”https://hohmature.news/wp-content/uploads/2023/09/jmHxTqYhe8m1bTrPQJnvY8odf8gsq1y1Q0i6Wp6Y.jpg”,”twitter_username”:null,”sort_order”:0,”created_at”:”2021-05-11T10:08:08.000000Z”,”updated_at”:”2022-08-03T17:04:41.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:17918,”author_id”:31,”sort_order”:1}}],”contentable”:{“id”:2900,”comments_open”:1,”created_at”:”2023-03-08T10:00:02.000000Z”,”updated_at”:”2023-04-13T15:22:45.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:13637,”model_type”:”AppModelsMarketingContent”,”model_id”:17918,”uuid”:”0af6ca4e-a1ee-4a7b-b9fb-a538b7d94695″,”collection_name”:”contents”,”name”:”24b364ff-eead-4160-9c1a-13890a2a4ad2″,”file_name”:”24b364ff-eead-4160-9c1a-13890a2a4ad2.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:283380,”manipulations”:[],”custom_properties”:{“alt”:”A high, overhead view looking down on a large crowd of tiny people and one tiny person standing alone in an empty, white, heart-shaped space “},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:13600,”created_at”:”2023-03-08T10:00:02.000000Z”,”updated_at”:”2023-03-08T10:00:11.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/13637/24b364ff-eead-4160-9c1a-13890a2a4ad2.jpg”}],”primary_content_topic”:{“id”:37,”name”:”Mind & Mood”,”slug”:”mind-and-mood”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/mind-and-mood”}},{“id”:18419,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Opill: Is this new birth control pill right for you?”,”short_title”:””,”subheading”:”Answers to key questions about the over-the-counter birth control pill approved by the FDA.”,”summary”:”n
The first nonprescription daily oral contraceptive was approved by the FDA earlier this year. Opill is expected to be available in early 2024. Here's what you should know about this new birth control pill.
n “,”content”:”
nn  n
n
n
Birth control pills have been safely used in the US (and sold only by prescription) for more than half a century. Just this past summer, the FDA approved Opill, the first daily contraceptive pill intended for sale over the counter. This offers many more people access to a new nonprescription option for preventing pregnancy.
n
Opill may be available early in 2024, although the exact date and cost are not yet known. Here’s what anyone interested — adults, parents, and teens — should know.
n
What is in Opill and how does it work?
n
Opill is a progestin-only form of birth control. That means it uses a single hormone called progestin (or norgestrel) to prevent pregnancy. It works by
n
- n
- affecting ovulation so that the ovaries do not release an egg every month
- thickening cervical mucus, which blocks sperm from reaching an egg
- changing the uterine lining in ways that keep a fertilized egg from implanting.
n
n
n
n
How effective is Opill at preventing pregnancy?
n
It depends on how consistent you are about taking Opill:
n
- n
- Perfect use means taking the pill every single day at the same time. With perfect use, Opill is 98% effective. That means that if 100 people take the medication perfectly, two or fewer people would become pregnant. Taking a pill perfectly can be difficult, though.
- Typical use averages how well a method works to prevent pregnancy when real people use it in real life. It considers that people sometimes use the pill inconsistently, like forgetting a dose or not taking it at the same time every day. With typical use, Opill is 91% effective. This means that if 100 people use Opill, but don’t take it perfectly, at least nine could become pregnant in a year.
n
n
n
It's also important to know that some medications make Opill less effective at preventing pregnancy. These include medicines used to treat migraines and seizures. Even though this birth control pill will be available over the counter, you should ask your health care provider if any medicines you take could make it less effective.
n
How do you take Opill?
n
- n
- Take it once a day at the same time each day until you finish the entire pack.
- Sticking to a consistent time of day, every day, is crucial. Timing matters with progestin-only pills like Opill because this medication works by raising progestin levels. However, progestin only stays elevated for 24 hours after you take each pill. After that, the progestin level will return to normal.
- After you complete a 28-day pack, you should immediately start a new pack of pills the next day.
n
n
n
n
What happens if you forget to take a dose at the specific time or miss a dose?
n
- n
- If you take the pill more than three hours late it will not be as effective at preventing pregnancy.
- Take the missed pill as soon you remember.
- You will need to use a backup birth control method such as condoms every time you have sex for the next 48 hours.
n
n
n
n
Is Opill safe for teenagers?
n
Opill is generally safe for most people who could get pregnant, including teenagers. There’s no evidence to suggest that safety or side effects are different in teenagers compared with adults.
n
Research done by the manufacturer has established the safety of Opill in people as young as 15 years old. It will be available without an age restriction.
n
When teens use birth control, what is the best choice for them?
n
There isn't a one-size-fits-all birth control method for all teenagers. The best method is the one a teen personally prefers and is committed to using consistently.
n
For teens who struggle with taking medication at the same time every day –– or anyone else who does –– Opill may not be the right choice. Fortunately, there are many options for preventing pregnancy, catering to individual preferences and goals.
n
Learn more about different contraception methods at the Center for Young Women’s Health website.
n
What side effects are common with Opill?
n
Progestin-only pills are usually associated with mild side effects. The most common side effects are:
n
- n
- unexpected vaginal bleeding or spotting
- acne
- headache
- gastrointestinal symptoms such as nausea, abdominal pain, and bloating
- change in appetite.
n
n
n
n
n
n
Opill does not cause problems with getting pregnant in the future, or cause cancer. Unlike birth control pills that combine the hormones estrogen and progestin, Opill will not increase the risk of a developing a blood clot.
n
Will Opill cause any mood changes?
n
Research looking at possible effects of progestin-only pills on mood is limited, so this is unclear. We do know that most people who take hormonal birth control methods do not experience negative mood changes.
n
Fortunately, there are many different types of effective birth control. If one method causes you unwanted side effects, talk to your health care provider. Together, you can figure out if another type of birth control may work better for you.
n
Can it be used as emergency birth control?
n
No, it should not be used as emergency birth control.
n
What should you know about STIs?
n
This type of birth control does not protect you from sexually transmitted infections (STIs) such as syphilis, gonorrhea, or chlamydia.
n
You can reduce the chance of getting STIs by correctly using condoms each time you have sex. There are different types of condoms: one made for penises and one made for vaginas.
n
Vaccines help protect against some STIs such as hepatitis B and human papillomavirus (HPV). A medicine called PrEP can help prevent HIV. Ask your medical team for more information about the right choices for you.
n
When will Opill be available and what will it cost?
n
The timeline for availability and the cost of medication is determined by the manufacturer. At time of FDA approval, it was expected to hit shelves in early 2024. No updates have been released for the exact date or estimated cost of the medication.
n “,”excerpt”:”n
The first nonprescription daily oral contraceptive was approved by the FDA earlier this year. Opill is expected to be available in early 2024. Here's what you should know about this new birth control pill.
n “,”short_excerpt”:”n
The first nonprescription daily oral contraceptive was approved by the FDA earlier this year. Opill is expected to be available in early 2024. Here's what you should know about this new birth control pill.
n “,”description”:null,”author”:null,”slug”:”opill-is-this-new-birth-control-pill-right-for-you-202311082989″,”sort_date”:”2023-11-08T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2989,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL110823″,”publication_date”:”2023-11-08T15:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-14T10:00:04.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-11-13T05:00:00.000000Z”,”active”:1,”created_at”:”2023-11-07T10:00:03.000000Z”,”updated_at”:”2023-11-14T10:00:04.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:46,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:474,”cr_id”:838,”featured”:0,”hhp_staff”:0,”hidden”:0,”name”:”Candice Mazon, MD”,”title”:null,”first_name”:”Candice”,”middle_name”:null,”last_name”:”Mazon”,”suffix”:”MD”,”slug”:”candice-mazon-md”,”byline”:”Contributor”,”description”:”
Dr. Candice Mazon is a second year adolescent medicine fellow at Boston Children's Hospital. She's a board certified pediatrician and received her training at MedStar Georgetown University Hospital. She earned her MD degree from Drexel University College of Medicine. Her interests include sexual health and reproductive justice, as well as addressing various health inequities.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/Ogerjm1yqEC3aCY8XysGOCpPbwDaK88HqOFofwog.jpg”,”twitter_username”:null,”sort_order”:0,”created_at”:”2023-11-06T18:45:44.000000Z”,”updated_at”:”2023-11-06T18:45:44.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18419,”author_id”:474,”sort_order”:1}},{“id”:475,”cr_id”:839,”featured”:0,”hhp_staff”:0,”hidden”:0,”name”:”Amy Desrochers DiVasta, MD, MMSc”,”title”:null,”first_name”:”Amy”,”middle_name”:”Desrochers”,”last_name”:”DiVasta”,”suffix”:”MD, MMSc”,”slug”:”amy-desrochers-divasta-md-mmsc”,”byline”:”Contributor”,”description”:”
Amy Desrochers DiVasta MD, MMSc, is chief of the division of adolescent medicine at Boston Children’s Hospital. She is the co-director of the adolescent long-acting reversible contraception program, and co-director of the reproductive endocrinology and PCOS program. Dr. DiVasta's research interests include the bone health of young women with low-estrogen states, such as girls with eating disorders, as well as reproductive health issues including long-acting contraception, PCOS, and endometriosis.
rnrn
Dr. DiVasta is also the co-scientific director for the Boston Center for Endometriosis, a joint project between Boston Children’s Hospital and Brigham and Women’s Hospital.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/nNkjO4OxGB16pAl5q3sHq30Cdje2Vy2mCA0a8N42.gif”,”twitter_username”:null,”sort_order”:0,”created_at”:”2023-11-06T22:06:13.000000Z”,”updated_at”:”2023-11-06T22:06:13.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18419,”author_id”:475,”sort_order”:2}}],”contentable”:{“id”:2989,”comments_open”:1,”created_at”:”2023-11-07T10:00:03.000000Z”,”updated_at”:”2023-11-07T10:00:03.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14494,”model_type”:”AppModelsMarketingContent”,”model_id”:18419,”uuid”:”7c0d1044-f18c-4f74-838c-4eecc2881928″,”collection_name”:”contents”,”name”:”ec54ca7d-b745-4ffb-8cf1-2b5ea1d438dd”,”file_name”:”ec54ca7d-b745-4ffb-8cf1-2b5ea1d438dd.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:122412,”manipulations”:[],”custom_properties”:{“alt”:”photo of a silver blister pack of birth control pills with the four rows of days of the week”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14440,”created_at”:”2023-11-07T10:00:03.000000Z”,”updated_at”:”2023-11-07T10:00:06.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14494/ec54ca7d-b745-4ffb-8cf1-2b5ea1d438dd.jpg”}],”primary_content_topic”:{“id”:46,”name”:”Women’s Health”,”slug”:”womens-health”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/womens-health”}},{“id”:18417,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Do children get migraine headaches? What parents need to know”,”short_title”:null,”subheading”:”A throbbing headache, nausea, and light sensitivity may be symptoms of migraine in children and teens”,”summary”:”
Headaches are very common in children and teens. We don’t tend to think about children getting migraines, but by age 10 one in 20 children has had one. Symptoms may differ from adults and it’s important for parents to understand triggers, helpful treatments, and possible red flags.
“,”content”:”

rnrn
Headaches are very common in children and teens. In fact, more than half will suffer from headaches at some point, and by 18 years the majority of adolescents have had them. And while most headaches are part of a viral illness, some are migraines. In fact, recurring migraines affect as many as one in 10 children and teens overall.
rnrn
What should you know — and do — if you think your child or teen may be having migraines?
rnrn
How early do migraines start to occur?
rnrn
We don't tend to think about migraines in children, but by age 10, one in 20 children has had a migraine. And migraines sometimes occur even earlier.
rnrn
Before puberty, boys and girls are equally likely to have them. After puberty, migraines are more common in girls.
rnrn
Which migraine symptoms are most common in children?
rnrn
Migraines are often one-sided in adults. In children they are more likely to be felt on both sides of the head, either in both temples or both sides of the forehead.
rnrn
While it's not always easy to tell a migraine from another kind of headache, children
rnrn
- rnt
- often report throbbing pain
- may experience nausea and sensitivity to light and noise.
rnt
rn
rnrn
The flashing lights and other vision changes people often see as a migraine begins are less common in children. However, parents may notice that their child is more tired, irritable, or pale before a migraine begins — and takes a while to get back to normal after it ends.
rnrn
What causes migraines in children?
rnrn
We don't know exactly what causes migraines. We used to think it had to do with blood flow to the brain, but that does not seem to be the case. It appears that migraines are caused by the nerves being more sensitive, and more reactive to stimulation. That stimulation could be stress, fatigue, hunger, almost anything.
rnrn
Migraines run in families. In fact, most migraine sufferers have someone in the family who gets migraines too.
rnrn
Can migraines be prevented?
rnrn
The best way to prevent migraines is to identify and avoid triggers. The triggers are different in each person, which is why it's a good idea to keep a headache diary.
rnrn
When your child gets a headache, write down what was happening before the headache, how badly it hurt and where, what helped, and anything else about it you can think of. This helps you and your doctor see patterns that can help you understand your child's particular triggers.
rnrn
It's a good idea to make sure your child gets enough sleep, eats regularly and healthfully, drinks water regularly, gets exercise, and manages stress. Doing this not only helps prevent migraines, but is also good for overall health!
rnrn
How can you help your child ease a migraine?
rnrn
When a migraine strikes, sometimes just lying down in a dark, quiet room with a cool cloth on the forehead is enough. If it's not, ibuprofen or acetaminophen can be helpful; your doctor can tell you the best dose for your child.
rnrn
It's important not to give your child these medications more than about 14 days a month, as giving them more often can lead to rebound headaches and make everything worse!
rnrn
Are there prescription medicines that can help children with migraines?
rnrn
If those approaches aren't enough, a class of medications called triptans can be helpful in stopping migraines in children ages 6 and up.
rnrn
If a child experiences frequent or severe migraines, leading to missed days of school or otherwise interfering with life, doctors often use medications to prevent migraines. There are a number of different kinds, and your doctor can advise you on what would be best for your child.
rnrn
Some girls get migraines around the time of their period. If that happens frequently, sometimes taking a prevention medicine around the time of menses each month can be helpful.
rnrn
When to contact your doctor
rnrn
If you think your child might be having migraines, you should call and make an appointment. Bring the headache diary with you. Your doctor will ask a bunch of questions, do a physical examination, and make a diagnosis. Together you can come up with the best plan for your child.
rnrn
You should always call your doctor, or go to an emergency room, if your child has a severe headache, a stiff neck, trouble with coordination or movement, is abnormally sleepy, or isn't talking or behaving normally.
rnrn
The American Academy of Pediatrics has additional useful information about migraines, and how to treat and prevent them, on their website.
“,”excerpt”:”
Headaches are very common in children and teens. We don’t tend to think about children getting migraines, but by age 10 one in 20 children has had one. Symptoms may differ from adults and it’s important for parents to understand triggers, helpful treatments, and possible red flags.
“,”short_excerpt”:”n
Headaches are very common in children and teens. We don’t tend to think about children getting migraines, but by age 10 one in 20 children has had one. Symptoms may differ from adults and it’s important for parents to understand triggers, helpful treatments, and possible red flags.
n “,”description”:null,”author”:null,”slug”:”do-children-get-migraine-headaches-what-parents-need-to-know-202311062988″,”sort_date”:”2023-11-06T05:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2988,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL110623″,”publication_date”:”2023-11-06T05:00:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-06T05:00:00.000000Z”,”last_import_type”:”insert”,”last_modified_date”:”2023-11-05T04:00:00.000000Z”,”active”:1,”created_at”:”2023-11-06T10:00:03.000000Z”,”updated_at”:”2023-11-08T21:43:11.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:24,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:46,”cr_id”:4,”featured”:0,”hhp_staff”:1,”hidden”:0,”name”:”Claire McCarthy, MD”,”title”:null,”first_name”:”Claire”,”middle_name”:null,”last_name”:”McCarthy”,”suffix”:”MD”,”slug”:”claire-mccarthy-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing”,”description”:”Claire McCarthy, MD, is a primary care pediatrician at Boston Children’s Hospital, and an assistant professor of pediatrics at Harvard Medical School. In addition to being a senior faculty editor for Harvard Health Publishing, Dr. McCarthy writes about health and parenting for Boston Children’s Hospital, Boston.com, and the Huffington Post.”,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/mvCBqecmOmDXOhy74hH3DviJmMAprZqhFgGbhTJL.jpg”,”twitter_username”:null,”sort_order”:5,”created_at”:”2021-05-11T10:23:17.000000Z”,”updated_at”:”2023-09-05T22:36:44.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18417,”author_id”:46,”sort_order”:1}}],”contentable”:{“id”:2988,”comments_open”:1,”created_at”:”2023-11-06T10:00:03.000000Z”,”updated_at”:”2023-11-08T21:43:11.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14489,”model_type”:”AppModelsMarketingContent”,”model_id”:18417,”uuid”:”af718b0f-65b7-4fc5-bd44-c8b03de827c8″,”collection_name”:”contents”,”name”:”cf914d00-e65a-4a1f-9d1d-146785bd94b1″,”file_name”:”cf914d00-e65a-4a1f-9d1d-146785bd94b1.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:90345,”manipulations”:[],”custom_properties”:{“alt”:”Brown-haired boy lying on colorful spread, looks pained, one hand covering an eye, other eye shut & other hand tucked behind head; concept is migraine headache”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14435,”created_at”:”2023-11-06T10:00:03.000000Z”,”updated_at”:”2023-11-06T10:00:12.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14489/cf914d00-e65a-4a1f-9d1d-146785bd94b1.jpg”}],”primary_content_topic”:{“id”:24,”name”:”Child & Teen Health”,”slug”:”child-and-teen-health”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/child-and-teen-health”}},{“id”:18039,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Does running cause arthritis?”,”short_title”:””,”subheading”:”Mounting evidence suggests the answer is no.”,”summary”:”n
It's easy to blame running when a person who runs regularly develops arthritis. But that blame may be misguided. Here's a look at the latest research on the topic.
n “,”content”:”
nn  n
n
n
When I took up running in college, a friend of mine scoffed at the idea. He hated running and was convinced runners were “wearing out” their joints. He liked to say he was saving his knees for his old age.
n
So, was he onto something? Does running really ruin your joints, as many people believe?
n
Runners can get arthritis, but is running the cause?
n
You may think the answer is obvious. Surely, years of running (pounding pavements, or even softer surfaces) could wear out your joints, much like tires wear out after you put enough miles on them. And osteoarthritis, the most common type of arthritis, usually affects older adults. In fact, it’s often described as age-related and degenerative. That sounds like a wear-and-tear sort of situation, right?
n
Maybe not. Sure, it’s easy to blame running when a person who runs regularly develops arthritis. But that blame may be misguided. The questions to ask are:
n
- n
- Does running damage the joints and lead to arthritis?
- Does arthritis develop first and become more noticeable while running?
- Is the connection more complicated? Perhaps there’s no connection between running and arthritis for most people. But maybe those destined to develop arthritis (due to their genes, for example) get it sooner if they take up running.
n
n
n
n
Extensive research over the last several decades has investigated these questions. While the answers are still not entirely clear, we’re moving closer.
n
What is the relationship between running and arthritis?
n
Mounting evidence suggests that that running does not cause osteoarthritis, or any other joint disease.
n
- n
- A study published in 2017 found that recreational runners had lower rates of hip and knee osteoarthritis (3.5%) compared with competitive runners (13.3%) and nonrunners (10.2%).
- According to a 2018 study, the rate of hip or knee arthritis among 675 marathon runners was half the rate expected within the US population.
- A 2022 analysis of 24 studies found no evidence of significant harm to the cartilage lining the knee joints on MRIs taken just after running.
n
n
n
n
These are just a few of the published medical studies on the subject. Overall, research suggests that running is an unlikely cause of arthritis — and might even be protective.
n
Why is it hard to study running and arthritis?
n
- n
- Osteoarthritis takes many years to develop. Convincing research would require a long time, perhaps a decade or more.
- It’s impossible to perform an ideal study. The most powerful type of research study is a double-blind, randomized, controlled trial. Participants in these studies are assigned to a treatment group (perhaps taking a new drug) or a control group (often taking a placebo). Double-blind means neither researchers nor participants know which people are in the treatment group and which people are getting a placebo. When the treatment being studied is running, there’s no way to conduct this kind of trial.
- Beware the confounders. A confounder is a factor or variable you can’t account for in a study. There may be important differences between people who run and those who don’t that have nothing to do with running. For example, runners may follow a healthier diet, maintain a healthier weight, or smoke less than nonrunners. They may differ with respect to how their joints are aligned, the strength of their ligaments, or genes that direct development of the musculoskeletal system. These factors could affect the risk of arthritis and make study results hard to interpret clearly. In fact, they may explain why some studies find that running is protective.
- The effect of running may vary between people. For example, it’s possible, though not proven, that people with obesity who run regularly are at increased risk of arthritis due to the stress of excess weight on the joints.
n
n
n
n
n
The bottom line
n
Trends in recent research suggest that running does not wear out your joints. That should be reassuring for those of us who enjoy running. And if you don’t like to run, that’s fine: try to find forms of exercise that you enjoy more. Just don’t base your decision — or excuse — for not running on the idea that it will ruin your joints.
n “,”excerpt”:”n
It's easy to blame running when a person who runs regularly develops arthritis. But that blame may be misguided. Here's a look at the latest research on the topic.
n “,”short_excerpt”:”n
It's easy to blame running when a person who runs regularly develops arthritis. But that blame may be misguided. Here's a look at the latest research on the topic.
n “,”description”:null,”author”:null,”slug”:”does-running-cause-arthritis-202304262930″,”sort_date”:”2023-04-26T04:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2930,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL042623″,”publication_date”:”2023-04-26T14:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-05-05T14:17:57.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-05-01T04:00:00.000000Z”,”active”:1,”created_at”:”2023-04-26T09:00:02.000000Z”,”updated_at”:”2023-05-05T14:17:57.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:10,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:23,”cr_id”:2,”featured”:1,”hhp_staff”:1,”hidden”:0,”name”:”Robert H. Shmerling, MD”,”title”:null,”first_name”:”Robert”,”middle_name”:”H.”,”last_name”:”Shmerling”,”suffix”:”MD”,”slug”:”robert-h-shmerling-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing”,”description”:”
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. As a practicing rheumatologist for over 30 years, Dr. Shmerling engaged in a mix of patient care, teaching, and research. His research interests center on diagnostic studies in patients with musculoskeletal symptoms, and rheumatic and autoimmune diseases. He has published research regarding infectious arthritis, medical ethics, and diagnostic test performance in rheumatic disease. Having retired from patient care in 2019, Dr. Shmerling now works as a senior faculty editor for Harvard Health Publishing.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/OdKCKaVzyx3xPsUxIBc9zJz8m3zvysnJa3UJsGOd.jpg”,”twitter_username”:”RobShmerling”,”sort_order”:4,”created_at”:”2021-05-11T10:05:10.000000Z”,”updated_at”:”2023-09-06T15:33:18.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18039,”author_id”:23,”sort_order”:1}}],”contentable”:{“id”:2930,”comments_open”:1,”created_at”:”2023-04-26T09:00:02.000000Z”,”updated_at”:”2023-04-28T02:33:12.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:13852,”model_type”:”AppModelsMarketingContent”,”model_id”:18039,”uuid”:”050facb4-31f0-4bc5-a423-53be3c108afd”,”collection_name”:”contents”,”name”:”2434e7c0-3082-4e6a-9556-3e36e6f38b4c”,”file_name”:”2434e7c0-3082-4e6a-9556-3e36e6f38b4c.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:63937,”manipulations”:[],”custom_properties”:{“alt”:”A middle-aged man wearing a blue zip top and lighter blue track pants running alongside a blurred cityscape”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:13810,”created_at”:”2023-04-26T09:00:02.000000Z”,”updated_at”:”2023-04-26T09:00:10.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/13852/2434e7c0-3082-4e6a-9556-3e36e6f38b4c.jpg”}],”primary_content_topic”:{“id”:10,”name”:”Exercise & Fitness”,”slug”:”exercise-and-fitness”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/exercise-and-fitness”}},{“id”:18415,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Long-lasting C. diff infections: A threat to the gut”,”short_title”:””,”subheading”:”Severe diarrhea and colon inflammation can persist for months — or years — after infection occurs due to gut microbiome imbalances.”,”summary”:”n
Virtually everyone carries the bacteria Clostridioides difficile, or C. diff. But half a million Americans a year develop a serious C. diff infection due to a gut microbiome imbalance. It disproportionately strikes people in hospitals and nursing homes, and can recur repeatedly.
n “,”content”:”
n  n
n
n
If you’ve ever dealt with diarrhea, you know how quickly it leaves you feeling depleted. Now imagine a case that rages on and on — or comes back again and again.
n
This is the reality for nearly 500,000 Americans each year who have the bacterial infection known as Clostridioides difficile, or C. diff. Virulent diarrhea and inflammation of the colon can even turn life-threatening.
n
This primer will help you understand how C. diff spreads and releases toxins, what the common symptoms are, and who is most vulnerable. Dr. Jessica Allegretti, director of the fecal microbiota program at Harvard-affiliated Brigham and Women’s Hospital, also touches on promising preventive strategies and treatments.
n
How does C. diff spread?
n
Like many bacteria, C. diff is present in our stool. It’s carried by virtually everyone — on our skin and even on the soles of our shoes. When C. diff bacteria are outside the body, they are inactive spores. They only have a chance to become active when they’re swallowed and reach the intestines.
n
Even then, many people who swallow C. diff spores never become ill. The spores only sicken people whose gut microbiome — the trillions of organisms living in their intestines — becomes imbalanced for one of the various reasons described below. When an imbalance occurs, the spores start to multiply and create toxins that lead to a C. diff infection.
n
“Many of us are colonized with C. diff bacteria without any consequences,” says Dr. Allegretti. “We’re swallowing C. diff spores all the time. Only under the right circumstances will the spores germinate and release a toxin. It’s the toxin that makes you sick.”
n
What are the symptoms of a C. diff infection?
n
The symptoms mimic those of many other types of gastrointestinal ailments. Initially, this may make it difficult to tell the infection apart from milder illnesses.
n
Symptoms to watch for include
n
- n
- persistent diarrhea lasting three or more days
- nausea
- fever
- stomach pain or tenderness
- appetite loss.
n
n
n
n
n
n
“C. diff isn’t something that people in the general population should be walking around scared of,” Dr. Allegretti says. “But if you need to take an antibiotic, be on the lookout for diarrheal symptoms after finishing the course of antibiotics. Diarrhea that’s associated with antibiotics alone should resolve once you finish taking the medication.”
n
Who is most vulnerable?
n
A few sobering facts from the Centers for Disease Control (CDC):
n
- n
- C. diff is the top cause of health care-associated infections in the US.
- It disproportionately strikes people in hospitals and nursing homes.
- Among people over 65, one in 11 of those diagnosed with a health care-associated case of C. diff dies within a month.
n
n
n
n
However, other groups are also susceptible to the infection. Health care-associated C. diff infections are plateauing, Dr. Allegretti notes, while so-called community-based infections that occur among the general population are increasing.
n
People most likely to experience such infections:
n
- n
- Are taking antibiotics or have just finished a course of antibiotic therapy. People are up to 10 times more likely to get C. diff while on antibiotics or during the month afterward, according to the CDC. “Not everyone who takes an antibiotic gets C. diff, and not everyone who gets C. diff gets recurrent C. diff,” says Dr. Allegretti. “It has a lot to do with your host response, your gut microbiome, and your individual risk factors, such as immunosuppression or inflammatory bowel disease.”
- Have a weakened immune system due to cancer, organ transplant, or treatment with immunosuppressive drugs (such as people with inflammatory bowel disease or autoimmune conditions).
- Have close contact with someone who has been diagnosed with C. diff.
n
n
n
n
What prevention strategies help block the spread of C. diff?
n
Hospitals try to prevent C diff. among patients in several ways. They impose scrupulous hand-washing requirements among staff members. Patients who develop new diarrhea are tested for C. diff infection. Those who have it are isolated in their own rooms to help prevent further spread.
n
Outside of a hospital, you can help prevent this gut infection through a few commonsense measures.
n
- n
- Wash your hands thoroughly with soap and water every time you use the bathroom and always before eating. Clean hands are especially important if you’ve had C. diff or know you’ve been exposed to someone with it. By the way, alcohol-based hand sanitizer isn’t effective against C. diff because its organisms can form resistant spores.
- Take antibiotics only when strictly necessary and for the shortest period possible. “The biggest thing we can do is advocate for ourselves,” Dr. Allegretti says. “During cold and flu season, we know a lot of unnecessary antibiotic prescriptions are written for infections that are most likely viral, not bacterial. Antibiotics do not kill viruses — and unnecessary antibiotics may upset the bacterial balance in your gut. Ask your doctor: Do I need this prescription? Is there an alternative?”
- When you do need antibiotics, ask if a narrow-spectrum antibiotic would be effective for your type of infection. Why? Broad-spectrum antibiotics kill a wider array of bacteria. This may be overkill, depleting your gut microbiome unnecessarily and enabling C. diff bacteria to germinate. “The caveat is, we don’t want patients to not take antibiotics they need for an actual infection,” she says. “But have a conversation with your health care team.”
n
n
n
n
The type of antibiotic prescribed also matters, according to a 2023 study in the journal Open Forum Infectious Diseases. Researchers compared more than 159,000 people who had C. diff infection with 797,000 healthy controls. Study findings suggest that using clindamycin and later-generation cephalosporin antibiotics pose the greatest risk for C. diff infection. Meanwhile, the antibiotics minocycline and doxycycline were associated with the lowest risk.
n
“But there are very few safe antibiotics with regard to C. diff risk,” Dr. Allegretti says.
n
Can probiotics help prevent or treat C. diff infection?
n
Probiotics are live microorganisms that can help keep the gut healthy and are found in supplements, yogurt, and other fermented foods. Two familiar examples are various strains of Lactobacillus and Bifidobacterium.
n
However, probiotics haven’t been found to prevent C. diff or its recurrence. Research performed in mice and humans suggests that giving probiotics after a course of antibiotics may slow the pace of microbiome recovery. “You’re potentially delaying the recovery of your microbiome with probiotics,” she says.
n
How is C. diff infection treated?
n
Ironically, C. diff therapy typically starts with antibiotics, despite the infection’s proliferation due to antibiotic use. The antibiotics of choice include fidaxomicin or oral vancomycin.
n
However, about one in five people will suffer one or more recurrences –– and with each one, yet another recurrence becomes far likelier, Dr. Allegretti says. A repeat episode may happen because people haven’t disinfected their homes effectively. That leaves them open to reinfection with the same strain of C. diff while still vulnerable.
n
When C. diff recurs, fecal microbial transplants (FMT) are considered the gold standard treatment. FMT transplants fecal matter from a healthy donor into a patient’s gut, placing it there using an endoscope, enema, or within an oral capsule. This year, the FDA approved two live fecal microbiota products aimed at preventing recurrent C. diff infections.
n
“We haven’t gotten away from antibiotics yet to treat this disease,” says Dr. Allegretti. “But we have a lot of preventative strategies now. It’s certainly very exciting for people struggling with C. diff infections.”
“,”excerpt”:”n
Virtually everyone carries the bacteria Clostridioides difficile, or C. diff. But half a million Americans a year develop a serious C. diff infection due to a gut microbiome imbalance. It disproportionately strikes people in hospitals and nursing homes, and can recur repeatedly.
n “,”short_excerpt”:”n
Virtually everyone carries the bacteria Clostridioides difficile, or C. diff. But half a million Americans a year develop a serious C. diff infection due to a gut microbiome imbalance. It disproportionately strikes people in hospitals and nursing homes, and can recur repeatedly.
n “,”description”:null,”author”:null,”slug”:”long-lasting-c-diff-infections-a-threat-to-the-gut-202311012987″,”sort_date”:”2023-11-01T04:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2987,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL110123″,”publication_date”:”2023-11-01T14:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-11-01T09:00:03.000000Z”,”last_import_type”:”insert”,”last_modified_date”:”2023-10-31T04:00:00.000000Z”,”active”:1,”created_at”:”2023-11-01T09:00:03.000000Z”,”updated_at”:”2023-11-01T09:00:04.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:28,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:420,”cr_id”:779,”featured”:0,”hhp_staff”:0,”hidden”:0,”name”:”Maureen Salamon”,”title”:null,”first_name”:”Maureen”,”middle_name”:null,”last_name”:”Salamon”,”suffix”:null,”slug”:”maureen-salamon”,”byline”:”Executive Editor, Harvard Women's Health Watch“,”description”:”
Maureen Salamon is executive editor of Harvard Women’s Health Watch. She began her career as a newspaper reporter and later covered health and medicine for a wide variety of websites, magazines, and hospitals. Her work has appeared in The New York Times, The Atlantic, CNN.com, WebMD, Medscape and HealthDay, among other major outlets. Maureen earned a BA in print journalism from Penn State University.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/MWQyHwiFAPooqhDKsjTfFjCCCoIooqQNLj1M7LRO.jpg”,”twitter_username”:null,”sort_order”:0,”created_at”:”2022-02-24T21:39:38.000000Z”,”updated_at”:”2022-07-17T15:04:53.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18415,”author_id”:420,”sort_order”:1}}],”contentable”:{“id”:2987,”comments_open”:1,”created_at”:”2023-11-01T09:00:03.000000Z”,”updated_at”:”2023-11-01T09:00:03.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14485,”model_type”:”AppModelsMarketingContent”,”model_id”:18415,”uuid”:”1b736cad-d2cc-4242-874e-bf8e2ef87c34″,”collection_name”:”contents”,”name”:”39724b9a-bb07-43dc-9f0d-ad6badb52175″,”file_name”:”39724b9a-bb07-43dc-9f0d-ad6badb52175.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:100859,”manipulations”:[],”custom_properties”:{“alt”:”Gloved fingers holding lab dish with red scratches and dots of bacteria on clear growing media; concept is testing for C. diff “},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14431,”created_at”:”2023-11-01T09:00:04.000000Z”,”updated_at”:”2023-11-01T09:00:05.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14485/39724b9a-bb07-43dc-9f0d-ad6badb52175.jpg”}],”primary_content_topic”:{“id”:28,”name”:”Diseases & Conditions”,”slug”:”diseases-and-conditions”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/diseases-and-conditions”}},{“id”:18413,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”How much sleep do you actually need?”,”short_title”:””,”subheading”:”Sleep quality counts as much as hours logged.”,”summary”:”n
Just how many hours of sleep are enough for you? The answer varies and it might be better to track sleep quality than focus on the number of hours you log each night.
n “,”content”:”
n  n
n
n
On average, how many hours do you sleep each night? For most healthy adults, guidelines suggest at least seven hours of slumber.
n
But these are general recommendations and not strict rules. “Some people need less than seven hours, while others might need more,” says Eric Zhou with the Division of Sleep Medicine at Harvard Medical School.
n
Do you need more or less sleep time?
n
We get it: you know people who swear they only need five hours of sleep per night, yet you feel foggy unless you log in eight to nine hours. The major reason for individual differences is that we often look at sleep the wrong way.
n
“Instead of focusing exclusively on the number of hours we sleep per night, we should also consider our sleep quality,” says Zhou.
n
Sleep quality means how well you sleep during the night. Did you sleep straight through? Or did you have periods where you woke up? If so, did it take you a long time to fall asleep? How did you feel when you woke up?
n
“If you awaken refreshed and feel like you have the energy to get through your day, then I would worry less about the exact number of hours you’re sleeping,” says Zhou.
n
How does sleep quality affect your health?
n
Sleep quality is vital for our overall health. Research has shown that people with poor sleep quality are at a higher risk for diabetes, heart disease, stroke, and mental health issues like anxiety and depression.
n
And that’s not all. “Poor sleep also can increase daytime fatigue and make it more difficult to enjoy life,” says Zhou.
n
Yet it’s normal for people’s sleep patterns to change over time. “Many people are not going to sleep in their 50s and 60s exactly like they did in their 20s,” says Zhou.
n
Many of these changes are age-related. For instance, your circadian rhythm — which regulates many bodily functions, including our sleep-wake cycle — can naturally get disrupted over time. This means people spend less time each night in restorative slow-wave sleep.
n
Production of melatonin, the sleep hormone, also gradually declines with age. “As a result of these changes, when we get older we may start to wake up earlier than we did when we were younger, or wake up more frequently during the night,” says Zhou.
n
How can you track sleep quality?
n
How can you better understand the factors likely contributing to your sleep quality? One way is to keep a sleep diary where you track and record your sleep.
n
Every day, record the time you went to bed, how long it took you to fall asleep, whether you had any nighttime awakenings (and if so, how long you were awake), and at what time you woke up. Also, keep track of how you feel upon awakening and at the end of the day.
n
“After a week or two, review the information to see if you can identify certain patterns that may be affecting your sleep quality, then make adjustments,” says Zhou.
n
For example, if you have trouble falling asleep, go to bed half an hour later than usual but maintain the same wake-up time. “It is common for people struggling with their sleep to try to get more sleep by staying in bed longer, but this disrupts their sleep patterns and diminishes their sleep quality,” says Zhou.
n
Three key strategies to support the quality of your sleep
n
Other strategies that can help support good sleep quality include:
n
- n
- maintaining a consistent wake time, especially on weekends
- limiting daytime naps to 20 to 30 minutes, and at least six hours before the desired bedtime
- being physically active.
n
n
n
n
When it comes to sleep quality, consistency is vital. “People with good sleep quality often have a predictable sleep window where their sleep occurs,” says Zhou. “Good sleepers are likely to sleep around the same number of hours and stay asleep through the night.”
n
The bottom line on getting restful sleep
n
It’s unrealistic to expect perfect sleep every night. “If you have trouble sleeping one or two nights during the week, that can be related to the natural ebbs and flows of life,” says Zhou. “You may have eaten a big meal that day, drank too much alcohol while watching football, or had a stressful argument with someone. When tracking sleep quality, look at your overall sleep health week-to-week, not how you slept this Tuesday compared to last Tuesday.”
n
If you are doing all the right things for your sleep but still do not feel rested upon waking, talk to your doctor. This can help you rule out a sleep disorder like sleep apnea, or another health issue that can interfere with sleep such as acid reflux or high blood pressure. Other factors that can affect the quality of your sleep include taking multiple medicines, depression, anxiety, loneliness, and environmental changes like temperature, noise, and light exposure.
“,”excerpt”:”n
Just how many hours of sleep are enough for you? The answer varies and it might be better to track sleep quality than focus on the number of hours you log each night.
n “,”short_excerpt”:”n
Just how many hours of sleep are enough for you? The answer varies and it might be better to track sleep quality than focus on the number of hours you log each night.
n “,”description”:null,”author”:null,”slug”:”how-much-sleep-do-you-actually-need-202310302986″,”sort_date”:”2023-10-30T04:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2986,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL103023″,”publication_date”:”2023-10-30T14:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-10-27T09:00:03.000000Z”,”last_import_type”:”insert”,”last_modified_date”:”2023-10-26T04:00:00.000000Z”,”active”:1,”created_at”:”2023-10-27T09:00:03.000000Z”,”updated_at”:”2023-10-27T09:00:03.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:44,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:66,”cr_id”:434,”featured”:1,”hhp_staff”:0,”hidden”:0,”name”:”Matthew Solan”,”title”:null,”first_name”:”Matthew”,”middle_name”:null,”last_name”:”Solan”,”suffix”:null,”slug”:”matthew-solan”,”byline”:”Executive Editor, Harvard Men's Health Watch“,”description”:”
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s Women Nutrition Connection and Women’s Health Advisor. Matthew’s articles on medicine, exercise science, and nutrition have appeared in Men’s Health, Men’s Fitness, Muscle & Fitness, Runner’s World, and Yoga Journal. He earned a master of fine arts in writing from the University of San Francisco and a bachelor of science in journalism from the University of Florida.
“,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/meFkQGpweKNzK8THXHlIORQI3ZZ68ShyfSRQykZN.jpg”,”twitter_username”:null,”sort_order”:0,”created_at”:”2021-05-11T10:26:17.000000Z”,”updated_at”:”2022-08-03T16:49:53.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18413,”author_id”:66,”sort_order”:1}}],”contentable”:{“id”:2986,”comments_open”:1,”created_at”:”2023-10-27T09:00:03.000000Z”,”updated_at”:”2023-10-27T09:00:03.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:14476,”model_type”:”AppModelsMarketingContent”,”model_id”:18413,”uuid”:”a1e8eaa0-2138-44a4-ada3-5ac5a54be159″,”collection_name”:”contents”,”name”:”266d658e-36d0-4ae5-b500-b20c187947cc”,”file_name”:”266d658e-36d0-4ae5-b500-b20c187947cc.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:47004,”manipulations”:[],”custom_properties”:{“alt”:”Happy white and black-faced sheep clustered around a big gray alarm clock; crescent moon and clouds against lilac background, concept sleep”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:14422,”created_at”:”2023-10-27T09:00:03.000000Z”,”updated_at”:”2023-10-27T09:00:06.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/14476/266d658e-36d0-4ae5-b500-b20c187947cc.jpg”}],”primary_content_topic”:{“id”:44,”name”:”Staying Healthy”,”slug”:”staying-healthy”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/staying-healthy”}},{“id”:18040,”content_source_id”:2,”content_type_id”:18,”content_access_type_id”:1,”title”:”Lead poisoning: What parents should know and do”,”short_title”:””,”subheading”:”Reports of defective tests put lead poisoning — and ways to prevent it — back in the spotlight.”,”summary”:”n
Lead poisoning is a serious health risk for children. And yet, they may be exposed to lead in their daily lives. Learn the dangers of lead exposure and what you can do to keep your child safe.
n “,”content”:”
nn  n
n
n
You may have heard recent news reports about a company that knowingly sold defective lead testing machines that tested tens of thousands of children between 2013 and 2017. Or wondered about lead in tap water after the widely reported problems with lead-contaminated water in Flint, Michigan. Reports like these are reminders that parents need to be aware of lead — and do everything they can to keep their children safe.
n
How is lead a danger to health?
n
Lead is poisonous to the brain and nervous system, even in small amounts. There really is no safe level of lead in the blood. We particularly worry about children under the age of 6. Not only are their brains actively developing, but young children commonly touch lots of things — and put their hands in their mouths. Children who are exposed to lead can have problems with learning, understanding, and behavior that may be permanent.
n
How do children get exposed to lead?
n
In the US, lead used to be far more ubiquitous than it is now, particularly in paint and gas. Yet children can be exposed to lead in many ways.
n
- n
- Lead paint. In houses built before 1978, lead paint can sometimes be under other paint, and is most commonly found on windowsills or around doors. If there is peeling paint, children can sometimes ingest it. Dust from old paint can land on the floor or other surfaces that children touch with their hands (and then put their hands in their mouths). If there was ever lead paint on the outside of a house, it can sometimes be in the dirt around a house.
- Leaded gas. While leaded gas was outlawed in 1996, its use is still allowed in aircraft, farm equipment, racing cars, and marine engines.
- Water passing through lead pipes. Lead can be found in the water of older houses that have lead pipes.
- Other sources. Lead can also be found in some imported toys, candles, jewelry, and traditional medicines. Some parents may have exposure at work or through hobbies and bring it home on their hands or clothing. Examples include working in demolition of older houses, making things using lead solder, or having exposure to lead bullets at a firing range.
n
n
n
n
n
What can parents do to protect children from lead?
n
First, know about possible exposures.
n
- n
- If you have an older home, get it inspected for lead if you haven’t done so already. (If you rent, federal law requires landlords to disclose known lead-based paint hazards when you sign a lease.) Inspection is particularly important if you are planning renovations, which often create dust and debris that increase the risk of exposure. Your local health department can give you information about how to do this testing. If there is lead in your home, don’t try to remove it yourself! It needs to be done carefully, by a qualified professional, to be safe.
- Talk to your local health department about getting the water in your house tested. Even if your house is new, there can sometimes be older pipes in the water system. Using a water filter and taking other steps can reduce or eliminate lead in tap water.
- If you have an older home and live in an urban area, there can be lead in the soil. You may want to have the soil around your house tested for lead. Don’t let your child play in bare soil, and be sure they take off their shoes before coming in the house and wash their hands after being outside.
- Learn about lead in foods, cosmetics, and traditional medications.
- Learn about lead in toys, jewelry, and plastics (yet another reason to limit your child’s exposure to plastic).
n
n
n
n
n
n
Second, talk to your pediatrician about whether your child should have a blood test to check for lead poisoning. The American Academy of Pediatrics recommends:
n
- n
- Assessing young children for risk of exposure at all checkups between 6 months and 6 years of age, and
- Testing children if a risk is identified, particularly at 12 and 24 months. Living in an old home, or in a community with lots of older homes, counts as a risk. Given that low levels of lead exposure that can lead to lifelong problems do not cause symptoms, it’s always better to be safe than sorry. If there is any chance that your child might have an exposure, get them tested.
n
n
n
How is childhood lead exposure treated?
n
If your child is found to have lead in their blood, the most important next step is to figure out the exposure — and get rid of it. Once the child is no longer exposed, the lead level will go down, although it does so slowly.
n
Iron deficiency makes the body more vulnerable to lead poisoning. If your child has an iron deficiency it should be treated, but usually medications aren’t used unless lead levels are very high. In those cases, special medications called chelators are used to help pull the lead out of the blood.
n
For more information, visit the Centers for Disease Control and Prevention website on lead poisoning prevention.
n “,”excerpt”:”n
Lead poisoning is a serious health risk for children. And yet, they may be exposed to lead in their daily lives. Learn the dangers of lead exposure and what you can do to keep your child safe.
n “,”short_excerpt”:”n
Lead poisoning is a serious health risk for children. And yet, they may be exposed to lead in their daily lives. Learn the dangers of lead exposure and what you can do to keep your child safe.
n “,”description”:null,”author”:null,”slug”:”lead-poisoning-what-parents-should-know-and-do-202305012931″,”sort_date”:”2023-05-01T04:00:00.000000Z”,”contentable_type”:”AppModelsMarketingBlogPost”,”contentable_id”:2931,”replacement_content_id”:null,”landing_page_landing_page_group_id”:null,”ucr_content_id”:”BL050123″,”publication_date”:”2023-05-01T14:30:00.000000Z”,”last_review_date”:null,”imported_at”:”2023-05-09T09:00:03.000000Z”,”last_import_type”:”update”,”last_modified_date”:”2023-05-08T04:00:00.000000Z”,”active”:1,”created_at”:”2023-04-29T09:00:02.000000Z”,”updated_at”:”2023-05-09T09:00:03.000000Z”,”deleted_at”:null,”images_remapped”:0,”old_product_id”:null,”old_content_id”:null,”hide_ads”:0,”primary_content_topic_id”:24,”ecommerce_type”:”CATALOG”,”authors”:[{“id”:46,”cr_id”:4,”featured”:0,”hhp_staff”:1,”hidden”:0,”name”:”Claire McCarthy, MD”,”title”:null,”first_name”:”Claire”,”middle_name”:null,”last_name”:”McCarthy”,”suffix”:”MD”,”slug”:”claire-mccarthy-md”,”byline”:”Senior Faculty Editor, Harvard Health Publishing”,”description”:”Claire McCarthy, MD, is a primary care pediatrician at Boston Children’s Hospital, and an assistant professor of pediatrics at Harvard Medical School. In addition to being a senior faculty editor for Harvard Health Publishing, Dr. McCarthy writes about health and parenting for Boston Children’s Hospital, Boston.com, and the Huffington Post.”,”image_url”:”https://d2icykjy7h7x7e.cloudfront.net/authors/mvCBqecmOmDXOhy74hH3DviJmMAprZqhFgGbhTJL.jpg”,”twitter_username”:null,”sort_order”:5,”created_at”:”2021-05-11T10:23:17.000000Z”,”updated_at”:”2023-09-05T22:36:44.000000Z”,”deleted_at”:null,”pivot”:{“content_id”:18040,”author_id”:46,”sort_order”:1}}],”contentable”:{“id”:2931,”comments_open”:1,”created_at”:”2023-04-29T09:00:02.000000Z”,”updated_at”:”2023-05-08T14:21:21.000000Z”,”deleted_at”:null,”media”:[]},”content_type”:{“id”:18,”name”:”blog”,”slug”:”blog”,”created_at”:”2021-05-11T08:30:32.000000Z”,”updated_at”:”2021-05-11T08:30:32.000000Z”,”deleted_at”:null},”media”:[{“id”:13853,”model_type”:”AppModelsMarketingContent”,”model_id”:18040,”uuid”:”746bd38a-930c-4882-8db8-61a9484b18c3″,”collection_name”:”contents”,”name”:”ffbadef4-72a7-4b93-9bb5-326d2c170b35″,”file_name”:”ffbadef4-72a7-4b93-9bb5-326d2c170b35.jpg”,”mime_type”:”image/jpeg”,”disk”:”s3″,”conversions_disk”:”s3″,”size”:60618,”manipulations”:[],”custom_properties”:{“alt”:”Peeling pieces of paint arranged to spell the word lead; concept is lead poisoning”},”generated_conversions”:{“micro”:true,”thumb”:true},”responsive_images”:[],”order_column”:13811,”created_at”:”2023-04-29T09:00:02.000000Z”,”updated_at”:”2023-04-29T09:00:11.000000Z”,”full_url”:”https://domf5oio6qrcr.cloudfront.net/medialibrary/13853/ffbadef4-72a7-4b93-9bb5-326d2c170b35.jpg”}],”primary_content_topic”:{“id”:24,”name”:”Child & Teen Health”,”slug”:”child-and-teen-health”,”is_primary”:1,”canonical”:”https://www.health.harvard.edu/topics/child-and-teen-health”}}], currentIndex: 0 }” x-on:slide-change.window=”currentIndex = $event.detail.currentIndex”>
Recent Blog Articles
Related Content
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!




