Dangerous complications from labor and delivery nearly doubled in Massachusetts between 2011 and 2020, according to a report released Wednesday by the Massachusetts Department of Public Health.
The complications, known as severe maternal morbidity, include unexpected and life-threatening events such as heart attacks, dangerously high blood pressure known as eclempsia, and extreme situations requiring life-saving interventions including the use of ventilators. Exacerbated by COVID-19 era delays in care, the complications disproportionately impact communities of color and people with disabilities, according to the report.
Analyzing the 678,382 deliveries that occurred in the Bay State between 2011 and 2020, researchers found that rates of severe maternal morbidity climbed from 52.3 per 10,000 deliveries in 2011 to 100.4 per 10,000 deliveries in 2020, an average increase of 8.9 percent each year
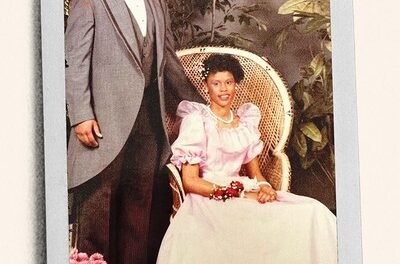
Although the rates increased for all populations during the 10-year period, women of color continue to face higher rates of complications, with Black women consistently experiencing the highest rates. Compared to white non-Hispanic women, Black non-Hispanic women experienced 2.3 times higher rates of complications on average during that time period, and Hispanic and Asian/Pacific Islander women experienced rates 1.2 times higher.
“The fact that these rates and the gaps have continued to worsen over time indicates that Black non-Hispanic birthing people have not benefited from improved medical knowledge and care,” said Dr. Hafsatou Diop, DPH’s Director of the Division of Maternal and Child Health Research and Analysis in a statement. “It has been long recognized that racism — not race — is the risk factor, as it leads to discriminatory beliefs and behaviors toward Black non-Hispanic birthing people.”
The data also showed evidence that the already-wide gap between white and Black women is growing. According to the report, the rate of complications among Black non-Hispanic women in 2020 was 2.5 times higher that than of white non-Hispanic women, a 25 percent increase from 2011, when there was a two-fold difference between the populations.
Rates were also found to increase with age, with complications highest among people 40 and older. Across ages, researchers note, Black non-Hispanic women had the highest rates of severe maternal morbidity. Black women aged 40 and older experienced by far the highest rates of any group: 238.6 per 10,000 deliveries.
The report also spotlighted troublingly high complication rates among people with disabilities. For every 10,000 deliveries, researchers found 131.6 instances of severe maternal morbidity among people with intellectual disabilities, 108.4 among those with impaired vision, and 94.6 among people with a disability that affects their mobility. Factors that drive higher rates of morbidity among people with disabilities “include active and passive denial of medical care, inequitable access to social determinants of health such as housing and proper nutrition, and higher rates of other risk factors such as smoking, stress, and clinically unwarranted obstetric intervention,” researchers wrote.
The findings reflect broader national trends. Earlier this year, a report from the Centers for Disease Control and Prevention found a sharp national increase in maternal deaths, which spiked by 40 percent between 2020 and 2021.
To address these issues, DPH is implementing several interventions, including a pilot program for remote blood pressure monitoring currently underway at Baystate Medical Center, Brigham and Women’s Hospital, and Boston Medical Center aimed at reducing serious complications caused by hypertensive disorders like eclempsia and preeclampsia, which are the leading cause for hospital readmission after labor.
It also supported the recommendations of a 2022 report by the Special Commission on Racial Inequities in Maternal Health, charged with investigating and studying methods to reduce racial inequities in maternal health in Massachusetts. These include creating legislation expanding access to doula and midwifery care, improved mental health and housing support, and diversifying the perinatal workforce.
The Massachusetts Moms Matter Act is one bill that would help the state move toward these goals. The legislation, which would establish two grant programs to expand and diversify the perinatal mental health workforce and invest in community programs supporting the mental wellbeing of new parents, was heard Monday by the Joint Committee on Mental Health, Substance Use, and Recovery.
Zeina Mohammed can be reached at zeina.mohammed@globe.com. Follow her on Twitter @_ZeinaMohammed.