November 13, 2023
2 min read
Key takeaways:
- Health-related quality of life measures were worse for adults with heart failure vs. those with several cancers.
- Data suggest clinicians should prioritize mental and physical health in HF care.
PHILADELPHIA — Older adults with heart failure have worse physical and mental health than those with several types of cancer, a speaker reported at the American Heart Association Scientific Sessions.
The data, from a pooled analysis of Medicare Advantage beneficiaries from 2016 to 2020, underscore the importance of prioritizing evidence-based interventions to improve physical and mental health in people with HF and to increase the use of guideline-recommended multidisciplinary clinics, according to Faraz Ahmad, MD, MS, FAHA, FACC, FHFSA, assistant professor of medicine at the Northwestern University Feinberg School of Medicine.
Data were derived from Shah K, et al. Abstract MDP299. Presented at: American Heart Association Scientific Sessions; Nov. 11-13, 2023; Philadelphia.
“As a community of clinicians taking care of people with HF, we need to prioritize discussing physical and mental health with our patients as a core component of patient-centered care,” Ahmad told Healio. “We also need to develop best practices to increase the measurement of patient-reported outcomes in clinical practice and implementing therapies and care delivery systems to prioritize the improvement of physical and mental health.”

Faraz Ahmad
In a pooled analysis, Ahmad and colleagues analyzed data from 71,025 adults aged 65 years and older with a self-reported history of HF, and older adults receiving active treatment for lung cancer (n = 4,165), colon cancer (n = 4,270), breast cancer (n = 14,542) or prostate cancer (n = 17,670), using Medicare Health Outcomes Survey data from 2016 to 2020.
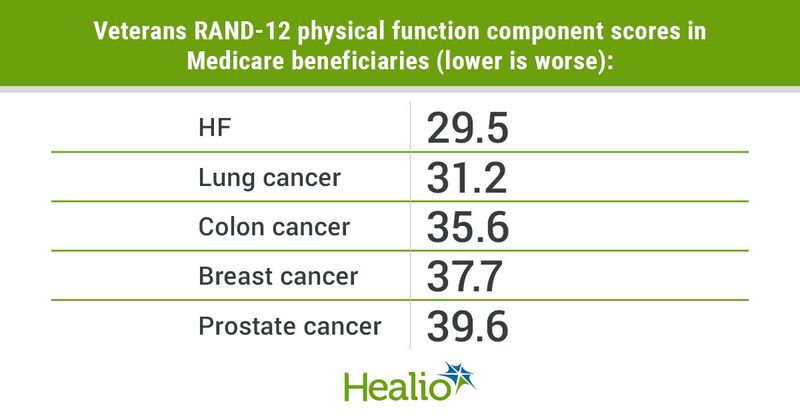
Researchers assessed the Veterans RAND-12 physical component score and mental component score, which range from 0 to 100 with a mean score of 50 and compared scores between patient groups.
The findings were simultaneously published in JACC: Heart Failure.
Among participants with HF (54% women; 16% Black), mean physical component score was 29.5, which is more than 2 standard deviations lower than in the U.S. general population. Mean mental component score was 47.9, which was also slightly lower than the U.S. general population.
Mean physical component score was lower among people with HF compared with adults with lung (31.2), colorectal (35.6), breast (37.7), and prostate cancer (39.6; P < .001 for all comparisons).
Participants with HF had a significantly lower mean mental component score than those with lung (49.5), colon (50), breast (52) and prostate (53) cancer (P < .001 for all comparisons).
“One area of important research is identifying best practices for routinely collecting patient-reported outcomes as part of HF care and then for how to best use these data as part of patient-centered care to improve the quality of life and longevity of people with HF,” Ahmad told Healio. “Another important area of research is using implementation science approaches to study and scale evidence-based interventions and multidisciplinary care delivery systems that target the improvement quality of life.”
Reference:
Sources/Disclosures
Collapse
Shah K, et al. Abstract MDP299. Presented at: American Heart Association Scientific Sessions; Nov. 11-13, 2023; Philadelphia.
Disclosures:
The authors report no relevant financial disclosures.