Abstract
To investigate the prevalence of multimorbidity and complex multimorbidity and their association with sociodemographic and health variables in individuals with severe obesity. This is a baseline data analysis of 150 individuals with severe obesity (body mass index ≥ 35.0 kg/m2) aged 18–65 years. The outcomes were multimorbidity and complex multimorbidity. Sociodemographic, lifestyle, anthropometric and self-perceived health data were collected. Poisson multiple regression was conducted to identify multimorbidity risk factors. The frequency of two or more morbidities was 90.7%, three or more morbidities was 76.7%, and complex multimorbidity was 72.0%. Living with four or more household residents was associated with ≥ 3 morbidities and complex multimorbidity. Fair and very poor self-perceived health was associated with ≥ 2 morbidities, ≥ 3 morbidities and complex multimorbidity. A higher BMI range (45.0–65.0 kg/m2) was associated with ≥ 2 morbidities and ≥ 3 morbidities. Anxiety (82.7%), varicose veins of lower limbs (58.7%), hypertension (56.0%) were the most frequent morbidities, as well as the pairs and triads including them. The prevalence of multimorbidity and complex multimorbidity in individuals with severe obesity was higher and the risk for multimorbidity and complex multimorbidity increased in individuals living in households of four or more residents, with fair or poor/very poor self-perceived health and with a higher BMI.
Introduction
Severe obesity (class II and III obesity) is a public health problem. Its prevalence has been increasing in an alarming rate worldwide. A study carried out in the United States projected that nearly 1 in 4 adults will have severe obesity by 2030 (24.2%; 95% CI 22.9 to 25.5) and its prevalence will reach more than 25%1. Another study in Spain found that 3.9% of adults suffered from class II obesity and over, affecting 1.32 million people2. In Brazil, 8.9 million adults had severe obesity in 2014 and its prevalence in women was 5.3% and in men 3.8%3.
In addition to the negative health impacts in individuals, severe obesity is often associated with several other morbidities4, especially a cardiometabolic cluster including hypertension, dyslipidemia, and diabetes5,6. In individuals with severe obesity, besides the elevated occurrence of cardiometabolic morbidities, osteoarticular and mental health problems are highly prevalent5. Among these, the most common are depression7 and anxiety8, highlighting that severe obesity is accompanied by a complex health scenario5.
In this context, the study of multimorbidity, that is, the presence of two or more morbidities in the same individual9,10, is important for this population, especially regarding the assessment of which morbidities occur more frequently in individuals with obesity5,11,12. This information is essential to the potential clinical interrelationship among morbidities and, consequently, to the associated pharmacological and non-pharmacological treatment approaches in this context13.
The concept of complex multimorbidity has been used to define the co-occurrence of three or more chronic conditions that affect three or more different body systems or different domains. This construct leads to lower prevalence compared to the traditional definition of multimorbidity, and is argued that it may also identify higher-need patients that demand care from different health providers14. Coordinating health care among the various medical specialists is a critical issue, thus, assessing complex multimorbidity may enable disease management and health policy planning15. People with severe obesity (BMI ≥ 35 kg/m2) are at greater risk for several morbidities and that they may account for a high proportion of the healthcare workload. However, few investigations contemplate this population, making it difficult to obtain a more robust picture on this subject5,16. Thus, it is important to investigate complex multimorbidity in this population.
Previous studies17,18 have identified that some sociodemographic factors and lifestyle are associated with multimorbidity and complex multimorbidity such as age19, sedentary lifestyle20, socio-economic inequalities21, daily moderate intake of alcohol22. However, there are few studies that identified the sociodemographic characteristics involved, the prevalence, and the pattern of morbidities in individuals with severe obesity. Understanding these factors is important to provide an integrated care approach, mainly because these morbidities are interrelated in a complex way and need to be managed in a coordinated and timely manner23. Additionally, there are still few studies that assess beyond the co-occurrence of morbidities. Therefore, this study aimed to investigate the prevalence of multimorbidity and complex multimorbidity and their association with sociodemographic, lifestyle and health variables in individuals with severe obesity. We also aimed to identify the most frequent morbidities, pairs, and triads according to BMI class.
Results
We analyzed data from 150 individuals with severe obesity with mean BMI 46.1 (± 6.5) kg/m2 and mean number of morbidities of 4.4 (± 2.4). The frequency of two or more morbidities was 90.7% (95%CI 84.8–94.8) (n = 136), three or more morbidities was 76.7% (95%CI 69.1–83.2) (n = 115), and complex multimorbidity was 72.0% (95%CI 64.7–79.2) (n = 108).
The mean age was 39.6 (± 8.8) years while the predominant age group was 35–44 years (44.0%), 85.3% were women, and 55.3% had brown skin color. Considering education and professional status, 67.3% had 9 or more years of schooling, 51.1% had lower per capita family income, and 68.7% were working in formal/informal/self-employed jobs. In addition, 52.0% lived in households with 4 or more residents, 67.3% reported never smoking, 70.2% had no binge drinking episodes in the last year, and 41.3% reported fair self-perceived health. Age group was associated with ≥ 3 morbidities, while household residents’ number, health self-perception, and BMI range were associated with ≥ 2 and ≥ 3 morbidities and also with complex multimorbidity (Table 1).
After adjustment in multiple regression analysis, living with four or more household residents was associated with ≥ 3 morbidities (PR: 1.31, 95%CI 1.09–1.56), and complex multimorbidity (PR: 1.39, 95%CI 1.11–1.74). Fair self-perceived health was associated with ≥ 2 morbidities (PR: 1.28, 95%CI 1.07–1.52), ≥ 3 morbidities (PR: 1.45, 95%CI 1.09–1.92), and complex multimorbidity (PR: 1.54, 95%CI 1.04–2.29). The same was observed for poor/very poor self-perceived health (≥ 2 morbidities: PR: 1.29, 95%CI 1.08–1.54; ≥ 3 morbidities: PR: 1.60, 95%CI 1.21–2.12, complex multimorbidity (PR: 2.08, 95%CI 1.44–3.01). A greater BMI range (45.0–65.0 kg/m2) was associated to ≥ 2 morbidities (PR: 1.16, 95%CI 1.04–1.29) and ≥ 3 morbidities (PR: 1.29, 95%CI 1.08–1.54) (Table 2).
Anxiety (82.7%), varicose veins of lower limbs (58.7%) and hypertension (56.0%) were the most frequent morbidities, followed by dyslipidemia (44.8%) and depression (31.3%). The combination of anxiety-hypertension (51.3%), anxiety-varicose veins of lower limbs (50.0%), and anxiety-dyslipidemia (36.7%) were the most common pairs of morbidities. Among triads of morbidities, anxiety-varicose veins of lower limbs-hypertension (31.3%), anxiety-hypertension-dyslipidemia (28.7%), and anxiety-varicose veins of lower limbs-dyslipidemia (22.0%) had the highest frequencies (Table 3).
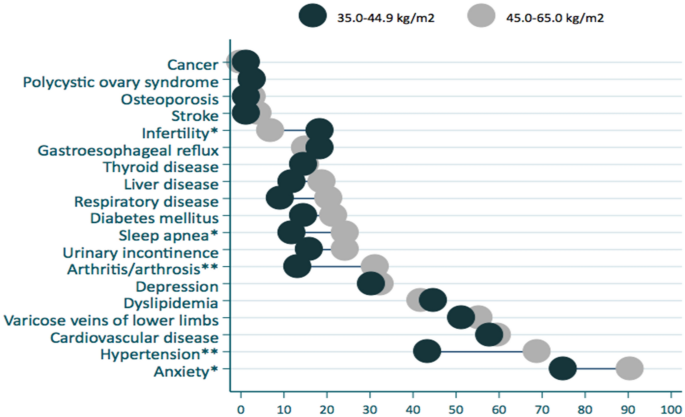
Individuals in the BMI range of 45.0 to 65.0 kg/m2 had significantly increased frequency of some morbidities compared to individuals with lower BMI (35.0 to 44.9 kg/m2), such as sleep apnea (24.3% vs. 11.8%, p < 0.05), arthritis/arthrosis (31.1% vs. 13.2%, p < 0.01), hypertension (68.9% vs. 43.4%, p < 0.01) and anxiety (90.5% vs. 75%, p < 0.05). For infertility the opposite was observed (26.3% vs. 73.7%, p < 0.05) (Fig. 1).
Discussion
Few studies have investigated complex multimorbidity in individuals with severe obesity. Our study provides valuable evidence for middle-income countries as few studies have investigated exclusively severe obesity and the co-occurrence of several morbidities and its associated factors in such context. Our results have shown that the prevalence of multimorbidity and complex multimorbidity in individuals with severe obesity are extremely high and the risk for multimorbidity has increased in individuals living in households of four or more residents, with fair or poor/very poor self-perceived health and with greater BMI. Additionally, we observed that cardiometabolic and mental health disorders were among the most frequent morbidities, such as hypertension, dyslipidemia, anxiety, and depression, as well as the combination of them. This scenario reveals the complex health status of individuals with severe obesity and the importance of developing clinical approaches capable of addressing not only the metabolic disorders, but also the mental health issues associated to severe obesity.
In the present study, we observed a high prevalence of multimorbidity (90.7% for two or more conditions and 76.7% for three or more conditions), as reported in other studies with individuals with severe obesity5,16. A Canadian study with 500 severely obese adults found 95.4% and 85.8% multimorbidity considering two and three chronic conditions, respectively5. Another study carried out in the United States, considering a list of 82 diseases, found a prevalence of 3 or more morbidities around 70% for obesity classes II and III24, which was similar to the present study. In the United Kingdom, results from a cohort demonstrated an increasing prevalence of multimorbidity as the BMI range rises, with emphasis on three times greater risk of ≥ 3 chronic conditions in individuals with BMI ≥ 40 kg/m2 compared to eutrophic individuals16. Divergences in the prevalence of multimorbidity are likely to be related to the use of different definitions of the outcome, the types and numbers of chronic conditions included in this assessment. Furthermore, the observation of greater risk of multimorbidity in higher degrees of obesity has been confirmed in several studies11,16,24,25,26. The inclusion of obesity in multimorbidity indices, sometimes left out, has been debated as a relevant point for epidemiological surveillance11. In this context, the importance of evaluating this outcome at higher levels of BMI is highlighted, given the exponential increase in severe obesity in recent years.
Age has been consistently associated with multimorbidity27, as the studies frequently report increasing prevalence with age27,28, and higher numbers in older persons compared (55–98%) to the whole population (20–30%)27. In our study, the prevalence of multimorbidity was higher in individuals aged 45–65 years (90%) when compared to 18–34 years (65.9%) only for ≥ 3 morbidities. We highlight the impact of severe obesity on the prevalence of multimorbidity demonstrated by the elevated estimates in the young adults with severe obesity in our study.
In this study, individuals with severe obesity living with four or more household residents had a higher risk of having three or more morbidities and complex multimorbidity. Data on family structure have shown that not living with children is associated with greater risk of multimorbidity29,30, however, investigations regarding the size of the family were not found. Family involvement has an important role in multimorbidity patient care, especially for the older adults. For younger individuals there is a lack of information regarding family structure and support in patient self-management of chronic diseases13,29. However, some negative experiences regarding the family involvement have been reported. Barriers to self-care (e.g. a family member refusal to eat the type of food the patient would like to eat) and responsibilities to multiple family members (multiple caregiver role) imposing competing demands on the patient’s time may result in poor self-management, nevertheless this topic is not clearly understood and needs further investigation31,32.
Concerning the health self-perception, in this study, the poor/very poor self-perceived health was associated with ≥ 2 morbidities, ≥ 3 morbidities, and complex multimorbidity. Several studies have demonstrated association of multimorbidity with fair and poor self-rated health in different populations, such as middle-aged and older individuals (OR = 3.4, 95% IC = 2.3–5.1)33, adults (PR = 3.70, 95% CI 2.73 to 5.00)34, older women35, Brazilian rural workers (OR 2.10, 95% CI 1.52–2.91)36, and persons aged 50 and older from 16 European nations (Adjusted OR = 2.13, 95% CI = 2.03–2.24)37. For complex multimorbidity, the same association was observed in Brazilian rural workers (OR 2.25, 95% CI 1.49–3.38)36.
Cardiometabolic morbidities are common in individuals with obesity6, resulting from excess body fat in different body regions, including the visceral region38. Varicose veins of lower limbs, hypertension and dyslipidemia were among the most frequent morbidities found in our sample, as expected. Concurrent cardiometabolic morbidities in this population collaborate to a higher risk of cardiovascular events, one of the major causes of death globally. The early identification of these outcomes contributes to the reduction of cardiovascular morbidity and mortality in individuals with obesity, especially severely obese ones6,39,40.
Another set of morbidities with common occurrence in obesity refers to mental health disorders, such as anxiety and depression41. Our results emphasize a high prevalence of anxiety and depression as they are among the most common morbidities, both alone and in pairs and triads. The high prevalence of mental health disorders in obesity could be attributed to both as a result of the disease itself, which carries a negative stigma for the individual, and as the multimorbidity associated with obesity42. Furthermore, individuals with multimorbidity may be at greater risk of developing or worsening mental health43,44. If not properly managed, mental health disorders may significantly interfere in the patient’s compliance with obesity and physical multimorbidity treatments, further worsening their health status45.
The present study has several strengths, such as its methodological quality and control during data collection; a wider list of morbidities/chronic conditions than previous studies that also used self-reported conditions; and the investigation of an important public health problem, such as severe obesity, that has been poorly investigated. As a potential limitation, we could mention the age range that did not include elderly individuals (> 65 years), and the use of self-reported data based on previous medical diagnosis. Despite many studies using this methodology to assess multimorbidity, and some self-reported information have been validated46,47, it may still present some bias, especially for mental health disorders48.
Our study has provided important data that could help improve prevention of diseases and healthcare of individuals with severe obesity. Multimorbidity, as a condition that affects populations across the world and, especially, people with obesity and severe obesity, has attracted the attention of researchers and clinicians. In this context, future studies should investigate multimorbidity applying weighted indexes that have been recently explored in some research. These indexes may provide a better understanding of the impact of multimorbidity on the functional status of individuals and enable tailored clinical decision-making, and guide interventions to maximize and preserve physical functioning.
Conclusion
Individuals with severe obesity had a high prevalence of multimorbidity and complex morbidity. Multimorbidity and complex multimorbidity were associated with living in households of four or more residents and fair or poor/very poor self-perceived health, while BMI of 45–65 kg/m2 was associated only with multimorbidity. The most common morbidities were cardiometabolic and mental health disorders, as well as the pairs and triads including them.
Methods
We analyzed baseline data of individuals with severe obesity from a randomized clinical trial entitled “Effect of Nutritional Intervention and Olive Oil in Severe Obesity: Randomized Controlled Trial-DieTBra Trial” (registered at ClinicalTrials.gov, NCT02463435). The research was conducted at the Clinical Research Unit (CRU) from Clinics Hospital, Federal University of Goiás, Goiânia, Goiás State, Brazil. We recruited individuals with BMI ≥ 35 kg/m2, aged 18 to 65 years old, and living in Goiânia and the metropolitan area. Exclusion criteria were to have already performed bariatric surgery, pregnancy, actual nutritional treatment for weight loss or in the previous 2 years, anti-obesity or anti-inflammatory drugs use, HIV/AIDS, heart/kidney/hepatic insufficiency, chronic obstructive pulmonary disease, and cancer. More detailed information on the DieTBra Trial can be found in previous publications6,49,50.
This study was approved by the Ethics Committee on Research with Humans of the Clinical Hospital/Federal University of Goiás under protocol number 747.792 and was conducted in accordance with the principles outlined in the Declaration of Helsinki. Informed consent was obtained from all participants included in the study, and the patient anonymity was preserved.
Structured questionnaires were tested and standardized in a pilot study for data collection. At baseline, we collected the following sociodemographic and health data: sex, age, schooling, per capita family income, marital status, skin color, work status, household number of residents, weight, height, BMI, smoking, alcohol consumption, health self-perception, and morbidities.
Participants’ body weight was measured to the nearest 0.05 kg using a calibrated digital scale (Welmy®) with capacity of 200 kg. Height was measured to the nearest 0.1 cm using a stadiometer. BMI (kg/m2) was calculated dividing the body mass (kg) by the squared height (m2). Severe obesity was defined as BMI ≥ 35 kg/m2 (NCD Risk Factor Collaboration, 2016).
Smoking habit was assessed by asking if the participant smoked or had ever smoked (cigarette, cigar, or pipe). Participants were classified as never smokers, former smokers, or current smokers. Alcohol consumption was assessed as binge drinking episodes (consumption of 5 or more drinks on at least 1 occasion) in the last year through an adapted version of the questionnaire of the Gender, Alcohol and Culture: An International Study (GENACIS) project51. Self-perceived health was assessed by asking: “In general, how do you rate your health: very good, good, fair, poor, or very poor?”52.
Multimorbidity was determined by a simple count of the following 19 self-reported morbidities: hypertension, cardiovascular disease (atherosclerosis, heart failure, heart attack), stroke, diabetes mellitus, dyslipidemia, anxiety, depression, sleep apnea, arthritis/arthrosis, gastroesophageal reflux, varicose veins of lower limbs, urinary incontinence, liver disease (fatty liver disease, cirrhosis), thyroid disease (hypothyroidism, hyperthyroidism), respiratory disease (asthma, bronchitis), cancer, infertility, polycystic ovary syndrome, and osteoporosis. In this study, we used the definition proposed by The European General Practice Research Network for multimorbidity as any combination of chronic disease with at least one other disease (acute or chronic) or biopsychosocial factor (associated or not) or somatic risk factor10, and we also analyzed the prevalence of 3 or more conditions. Complex multimorbidity was defined as the occurrence of three or more chronic conditions affecting three or more body systems or different domains14.
The sample size was calculated a posteriori using Epi Info 7 for many explanatory variables, which health self-perception had the highest value (n = 131) for the following parameters: 95% confidence level, 80% power, unexposed: exposed ratio of 33.3: 64.5 being the exposition the fair health self-perception, the percentage outcome in unexposed group 33.3% and risk ratio of 1.81. Therefore, the sample size of the clinical trial (n = 150) was sufficient to cover the purpose of this study.
Descriptive analyses were performed using absolute and relative frequencies, means and standard deviations. The frequency of top ten pairs and triads of morbidities were calculated to describe the most common combinations of conditions. The association between the outcome and independent variables was tested using Pearson’s Chi-squared test and Tendency Chi-squared test. Calculations of relative risks and their 95% confidence intervals (95% CI) were performed using Poisson regression with robust variance. The multiple regression model was adjusted for variables with a p-value < 0.20. The significance level was established at 5% (95% confidence level). All analyses were conducted using STATA 12.0®. Data entry was performed in duplicate for consistency check using EPI DATA® 3.1.
The study was approved by the Research Ethics Committee of the Clinics Hospital of the Federal University of Goiás (protocol number 747.792). All patients who agreed to participate signed an informed consent.
Data availability
We analyzed baseline data of individuals with severe obesity from a randomized clinical trial entitled “Effect of Nutritional Intervention and Olive Oil in Severe Obesity: Randomized Controlled Trial-DieTBra Trial” (registered at ClinicalTrials.gov, NCT02463435). The datasets used and/or analyzed during the current study are available upon formal request to author EA Silveira.
References
-
Ward, Z. J. et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N. Engl. J. Med. 381, 2440–2450. https://doi.org/10.1056/NEJMsa1909301 (2019).
-
Espallardo, O. The impact of severe obesity on healthcare resource utilisation in Spain. Obes. Surg. 27, 2058–2066 (2017).
-
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016(387), 1377–1396. https://doi.org/10.1016/S0140-6736(16)30054-X (2016).
-
Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 15, 288–298. https://doi.org/10.1038/s41574-019-0176-8 (2019).
-
Agborsangaya, C. B., Majumdar, S. R., Sharma, A. M., Gregg, E. W. & Padwal, R. S. Multimorbidity in a prospective cohort: Prevalence and associations with weight loss and health status in severely obese patients: Multimorbidity in severely obese patients. Obesity 23, 707–712. https://doi.org/10.1002/oby.21008 (2015).
-
Santos, A. S., Rodrigues, A. P. S., Rosa, L. P., Sarrafzadegan, N. & Silveira, E. A. Cardiometabolic risk factors and Framingham risk score in severely obese patients: Baseline data from DieTBra Trial. Nutr. Metab. Cardiovasc. Dis. 30, 474–482 (2020).
-
Stiglbauer, V. et al. Immunological substrates of depressive symptoms in patients with severe obesity: An exploratory study. Cell Biochem. Funct. 39, 423–431. https://doi.org/10.1002/cbf.3608 (2021).
-
Gill, H. et al. The long-term effect of bariatric surgery on depression and anxiety. J. Affect. Disord. 246, 886–894. https://doi.org/10.1016/j.jad.2018.12.113 (2019).
-
Johnston, M. C., Crilly, M., Black, C., Prescott, G. J. & Mercer, S. W. Defining and measuring multimorbidity: A systematic review of systematic reviews. Eur. J. Public Health 29, 182–189 (2019).
-
Le Reste, J. Y. et al. The European General Practice Research Network presents a comprehensive definition of multimorbidity in family medicine and long term care, following a systematic review of relevant literature. J. Am. Med. Dir. Assoc. 14, 319–325. https://doi.org/10.1016/j.jamda.2013.01.001 (2013).
-
Agborsangaya, C. B., Ngwakongnwi, E., Lahtinen, M., Cooke, T. & Johnson, J. A. Multimorbidity prevalence in the general population: The role of obesity in chronic disease clustering. BMC Public Health 13, 1161. https://doi.org/10.1097/GME.0b013e31827fdd8c (2013).
-
Flores, T. R. et al. The risk of multimorbidity associated with overweight and obesity: Data from the Brazilian National Health Survey 2013. J. Obes. Metab. Syndr. https://doi.org/10.7570/jomes20110 (2021).
-
Boyd, C. M. & Fortin, M. Future of multimorbidity research: How should understanding of multimorbidity inform health system design?. Public Health Rev. 32, 451–474. https://doi.org/10.1007/BF03391611 (2010).
-
Harrison, C., Britt, H., Miller, G. & Henderson, J. Examining different measures of multimorbidity, using a large prospective cross-sectional study in Australian general practice. BMJ Open 4, e004694. https://doi.org/10.1136/bmjopen-2013-004694 (2014).
-
Salisbury, C., Johnson, L., Purdy, S., Valderas, J. M. & Montgomery, A. A. Epidemiology and impact of multimorbidity in primary care: A retrospective cohort study. Br. J. Gen. Pract. 61, e12–e21. https://doi.org/10.3399/bjgp11X548929 (2011).
-
Booth, H. P., Prevost, A. T. & Gulliford, M. C. Impact of body mass index on prevalence of multimorbidity in primary care: Cohort study. Fam. Pr. 31, 38–43. https://doi.org/10.1093/fampra/cmt061 (2014).
-
Kone, A. P. et al. Rising burden of multimorbidity and related socio-demographic factors: A repeated cross-sectional study of Ontarians. Can. J. Public Health. 112, 737–747. https://doi.org/10.17269/s41997-021-00474-y (2021).
-
Larsen, F. B., Pedersen, M. H., Friis, K., Glümer, C. & Lasgaard, M. A latent class analysis of multimorbidity and the relationship to socio-demographic factors and health-related quality of life. A national population-based study of 162,283 Danish adults. PLoS ONE 12, e0169426. https://doi.org/10.1371/journal.pone.0169426 (2017).
-
Basham, C. A. Multimorbidity prevalence in Canada: A comparison of northern territories with provinces, 2013/14. Int. J. Circumpolar Health 78, 1607703 (2019).
-
Lear, S. A. et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet. 390(10113), 2643–2654 (2017).
-
Chan, M. S. et al. Socio-economic inequalities in life expectancy of older adults with and without multimorbidity: A record linkage study of 1.1 million people in England. Int. J. Epidemiol. 48, 12 (2019).
-
Sakib, M. N., Shooshtari, S., St. John, P. & Menec, V. The prevalence of multimorbidity and associations with lifestyle factors among middle-aged Canadians: An analysis of Canadian longitudinal study on aging data. BMC Public Health 19, 243. https://doi.org/10.1186/s12889-019-6567-x (2019).
-
Violan, C. et al. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS ONE 9, e102149. https://doi.org/10.1371/journal.pone.0102149 (2014).
-
Madlock-Brown, C. R., Reynolds, R. B. & Bailey, J. E. Increases in multimorbidity with weight class in the United States. Clin. Obes. 11, e12436 (2021).
-
Botoseneanu, A. et al. Multimorbidity accumulation among middle-aged Americans: Differences by race/ethnicity and body-mass index. J. Gerontol. Biol. Sci. Med. Sci. https://doi.org/10.1093/gerona/glab116 (2021).
-
Kivimäki, M. et al. Body-mass index and risk of obesity-related complex multimorbidity: An observational multicohort study. Lancet Diabetes Endocrinol. 10, 253–263 (2022).
-
Marengoni, A. et al. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 10, 430–439. https://doi.org/10.1016/j.arr.2011.03.003 (2011).
-
Cassell, A. et al. The epidemiology of multimorbidity in primary care: A retrospective cohort study. Br. J. Gen. Pract. 68, e245–e251. https://doi.org/10.3399/bjgp18X695465 (2018).
-
Agborsangaya, C. B., Lau, D., Lahtinen, M., Cooke, T. & Johnson, J. A. Multimorbidity prevalence and patterns across socioeconomic determinants: A cross-sectional survey. BMC Public Health 12, 201. https://doi.org/10.1186/1471-2458-12-201 (2012).
-
Taylor, A. W. et al. Multimorbidity—not just an older person’s issue. Results from an Australian Biomedical Study. BMC Public Health 10, 718. https://doi.org/10.1186/1471-2458-10-718 (2010).
-
Rosland, A.-M., Heisler, M., Choi, H.-J., Silveira, M. J. & Piette, J. D. Family influences on self-management among functionally independent adults with diabetes or heart failure: Do family members hinder as much as they help?. Chronic Illn. 6, 22–33. https://doi.org/10.1177/1742395309354608 (2010).
-
Samuel-Hodge, C. D. et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: Spirituality, the multi-caregiver role, and other social context factors. Diabetes Care 23, 928–933. https://doi.org/10.2337/diacare.23.7.928 (2000).
-
Mavaddat, N., Valderas, J. M., van der Linde, R., Khaw, K. T. & Kinmonth, A. L. Association of self-rated health with multimorbidity, chronic disease and psychosocial factors in a large middle-aged and older cohort from general practice: A cross-sectional study. BMC Fam. Pract. 15, 185. https://doi.org/10.1186/s12875-014-0185-6 (2014).
-
Araujo, M. E. A., Silva, M. T., Galvao, T. F., Nunes, B. P. & Pereira, M. G. Prevalence and patterns of multimorbidity in Amazon region of Brazil and associated determinants: A cross-sectional study. BMJ Open 8, e023398. https://doi.org/10.1136/bmjopen-2018-023398 (2018).
-
Vos, H. M. M., Bor, H. H., van Rangelrooij-Minkels, M. J. A., Schellevis, F. G. & Lagro-Janssen, A. L. M. Multimorbidity in older women: The negative impact of specific combinations of chronic conditions on self-rated health. Eur. J. Gen. Pract. 19, 117–122. https://doi.org/10.3109/13814788.2012.755511 (2013).
-
Petarli, G. B. et al. Multimorbidity and complex multimorbidity in Brazilian rural workers. PLoS ONE 14, e0225416. https://doi.org/10.1371/journal.pone.0225416 (2019).
-
Palladino, R., Tayu Lee, J., Ashworth, M., Triassi, M. & Millett, C. Associations between multimorbidity, healthcare utilisation and health status: Evidence from 16 European countries. Age Ageing 45, 431–435. https://doi.org/10.1093/ageing/afw044 (2016).
-
Zhang, J., Xu, L., Li, J., Sun, L. & Qin, W. Association between obesity-related anthropometric indices and multimorbidity among older adults in Shandong, China: A cross-sectional study. BMJ Open https://doi.org/10.1136/bmjopen-2019-036664 (2020).
-
Pollack, L. M. et al. Obesity-related multimorbidity and risk of cardiovascular disease in the middle-aged population in the United States. Prev. Med. 139, 106225 (2020).
-
Soriano-Maldonado, A., Aparicio, V. A., Felix-Redondo, F. J. & Fernandez-Berges, D. Severity of obesity and cardiometabolic risk factors in adults: Sex differences and role of physical activity. The HERMEX Study. Int. J. Cardiol. 223, 352–359 (2016).
-
Canheta, ABd. S., Santos, ASe. Ad. C., de Souza, J. D. & Silveira, E. A. Traditional Brazilian diet and extra virgin olive oil reduce symptoms of anxiety and depression in individuals with severe obesity: Randomized clinical trial. Clin. Nutr. 40, 404–411. https://doi.org/10.1016/j.clnu.2020.05.046 (2021).
-
Romain, A. J., Marleau, J. & Baillot, A. Association between physical multimorbidity, body mass index and mental health/disorders in a representative sample of people with obesity. J. Epidemiol. Community Health 73, 874–880 (2019).
-
Garin, N. et al. Global multimorbidity patterns: A cross-sectional, population-based, multi-country study. J. Gerontol. A. Biol. Sci. Med. Sci. 71, 205–214. https://doi.org/10.1093/gerona/glv128 (2016).
-
Gould, C. E., O’Hara, R., Goldstein, M. K. & Beaudreau, S. A. Multimorbidity is associated with anxiety in older adults in the health and retirement study: Multimorbidity and anxiety. Int. J. Geriatr. Psychiatry 31, 1105–1115. https://doi.org/10.1002/gps.4532 (2016).
-
Sarwer, D. B. & Polonsky, H. M. The psychosocial burden of obesity. Endocrinol. Metab. Clin. 45, 677–688 (2016).
-
Chrestani, M. A. D., dos Santos, Id. S. & Matijasevich, A. M. Hipertensão arterial sistêmica auto-referida: validação diagnóstica em estudo de base populacional. Cad. Saúde Pública 25, 2395–2406. https://doi.org/10.1590/S0102-311X2009001100010 (2009).
-
Lima-Costa, M. F., Peixoto, S. V., Firmo, J. O. A. & Uchoa, E. Validade do diabetes auto-referido e seus determinantes: evidências do projeto Bambuí. Rev. Saúde Pública 41, 947–953. https://doi.org/10.1590/S0034-89102007000600009 (2007).
-
Costa, E. et al. Prevalence of International Classification of Diseases, 10th revision common mental disorders in the elderly in a Brazilian community: The Bambui Health Ageing Study. Am. J. Geriatr. Psychiatry 15, 17–27. https://doi.org/10.1097/01.JGP.0000230659.72417.a0 (2007).
-
Rodrigues, APd. S., Rosa, L. P. S., da Silva, H. D., Silveira-Lacerda, Ed. P. & Silveira, E. A. The single nucleotide polymorphism PPARG2 Pro12Ala affects body mass index, fat mass, and blood pressure in severely obese patients. J. Obes. 2018, 1–9. https://doi.org/10.1155/2018/2743081 (2018).
-
Rodrigues, A. P. S., Rosa, L. P. S. & Silveira, E. A. PPARG2 Pro12Ala polymorphism influences body composition changes in severely obese patients consuming extra virgin olive oil: A randomized clinical trial. Nutr. Metab. 15, 52. https://doi.org/10.1186/s12986-018-0289-4 (2018).
-
Lima, M. C. P., Kerr-Côrrea, F. & Rehm, J. Alcohol consumption pattern and coronary heart disease risk in metropolitan São Paulo: Analyses of GENACIS project. Rev. Bras. Epidemiol. 16, 49–57 (2013).
-
Burkert, N. T., Freidl, W., Muckenhuber, J., Stronegger, W. J. & Rásky, É. Self-perceived health, quality of life, and health-related behavior in obesity: Is social status a mediator?. Wien. Klin. Wochenschr. 124, 271–275. https://doi.org/10.1007/s00508-012-0160-y (2012).
Acknowledgements
We would like to thank all study participants and undergraduate volunteers which participated in our study.
Funding
This study was partially funded by Fundação de Amparo à Pesquisa no Estado de Goiás (FAPEG) (grant number 201310267000003). This work was supported by the Economic and Social Research Council (ESRC) [grant number ES/T008822/1].
Author information
Authors and Affiliations
Contributions
Study concept and design: A.P.d.S.R. and E.A.S.; acquisition of data: A.P.d.S.R., A.S.A.S., A.B.d.S.C., A.T.d.O.R., C.d.O., and E.A.S.; analysis and interpretation of data: A.P.d.S.R., S.R.R.B., B.P.N., C.d.O.; drafting of the manuscript: A.P.d.S.R., A.S.A.S., A.B.d.S.C., S.R.R.B., A.T.d.O.R., C.d.O., and B.P.N.; critical revision of the manuscript: all authors; statistical analysis: A.P.d.S.R.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rodrigues, A.P.d., Batista, S.R.R., Santos, A.S.e. et al. Multimorbidity and complex multimorbidity in Brazilians with severe obesity.
Sci Rep 13, 16629 (2023). https://doi.org/10.1038/s41598-023-43545-5
-
Received:
-
Accepted:
-
Published:
-
DOI: https://doi.org/10.1038/s41598-023-43545-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.