Patients with psoriatic arthritis (PsA), rheumatoid arthritis (RA), or ankylosing spondylitis (AS) receiving golimumab reported consistently high retention rates when used as a first-line treatment, according to a study published in Clinical Rheumatology.1 Persistence was also high when used as a second-line treatment in patients with RA.
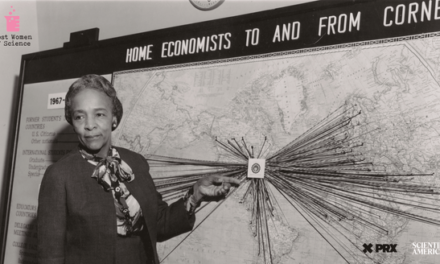
Cindy L J Weinstein, MD, PhD
Credit: ResearchGate

“Continuous therapeutic treatment is important in the context of chronic autoimmune diseases,” wrote lead investigator Cindy L J Weinstein, MD, PhD, senior director of clinical research at Merck, and colleagues. “Treatment persistence, or the total time from initiation to discontinuation of therapy, depends upon drug efficacy, patient satisfaction, safety, and tolerability and is therefore regarded as a useful measure of overall drug effectiveness.”
Additionally, suboptimal persistence can lead to higher disease activity, increased healthcare utilization, morbidity, and mortality.2
To better understand and characterize drug retention and discontinuation across patient groups, the post-hoc analysis assessed the 5-year persistence of golimumab, a monoclonal antibody against tumor necrosis factor-α (TNF-α), across studies, indications, and lines of therapy using log-rank tests. The probability of retention was estimated using a Kaplan-Meier analysis.
The drug was subcutaneously administered at doses of 50 or 100 mg every 4 weeks for up to 5 years. Using data from 5 phase 3, randomized, placebo-controlled clinical trials, a total of 2228 adult participants with PsA (GO-REVEAL study), AS (GO-RAISE study) and RA (GO-BEFORE, GO-AFTER, and GO-FORWARD studies) were included in the assessment. Of these patients, 1797 received golimumab as first-line therapy (RA = 1050; PsA = 394; AS = 353), while 431 patients with RA received the drug as second-line therapy.
Retention rates for golimumab treatment at the 5-year mark were consistently high when used as a first-line therapy (69.8%), which did not significantly differ across conditions (P = .5106) or first-line studies (P = .2327). Additionally, persistence was better in those who received the drug as first-line therapy compared with second-line therapy (41.6%).
Investigators pooled the 3 first-line RA studies to compare with the second-line study to better understand the differences between groups. Patients who received golimumab as a second-line therapy reported a longer disease duration compared with those receiving it as a first-line therapy (median 9.2 vs 3.7 years, respectively). They were also more likely to be female (78.7% vs 62.2%), older than 50 years (61.5% vs 41.2%), and have prior experience with corticosteroids (52.7% vs 41.3%) or methotrexate (66.1% vs 58.1%). The results may indicate disease duration was more impacted by line of therapy than by indication.
Investigators noted the disproportionate number of patients with RA as a limitation of the study, as it may have skewed baseline characteristics to favor more typical RA characteristics. This was mitigated by pooling the 3 first-line RA studies to compare with the second-line study. However, small subgroup sample sizes and differences in disease characteristics may have hindered the assessment of retention prediction. Lastly, as patients with PsA and AS were not included in the second-line therapy cohort, results may not be generalizable beyond patients with RA.
“Taken together, the present analysis supports the value of long-term golimumab use as first-line therapy in patients with rheumatic diseases (RA, PsA and AS) and as second-line therapy in patients with RA,” investigators concluded. “Factors affecting retention rates in different indications are not yet fully understood and would be an important topic for future investigation, particularly in large cohorts with long follow-up duration.”
References
- Weinstein CLJ, Meehan AG, Lin J, Briscoe SD, Govoni M. Long-term golimumab persistence: Five-year treatment retention data pooled from pivotal Phase III clinical trials in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis [published online ahead of print, 2023 Sep 26]. Clin Rheumatol. 2023;10.1007/s10067-023-06760-z. doi:10.1007/s10067-023-06760-z
- Harnett J, Wiederkehr D, Gerber R, Gruben D, Koenig A, Bourret J (2016) Real-world evaluation of TNF-inhibitor utilization in rheumatoid arthritis. J Med Econ 19:91–102. https://doi.org/10.3111/13696998.2015.1099538