Abstract
Older people spend most of their time indoors. Limited evidence demonstrates that exposure to indoor air pollutants might be related to chronic complications. This study aimed to estimate the correlation between household air pollution (HAP)’s long-term exposure and the prevalence of elevated hypertension, diabetes mellitus (DM), obesity, and low-density lipoprotein (LDL) cholesterol. From the Global Burden disease dataset, we extracted HAP, hypertension, DM, body mass index, and LDL cholesterol data from Iran from 1990 to 2019 to males and females in people over 50 years. We present APC and AAPC and their confidence intervals using Joinpoint Software statistical software. R software examined the correlation between HAP and hypertension, DM2, Obesity, and high LDL cholesterol. Our finding showed a significant and positive correlation between HAP exposure and prevalence of high low-density lipoprotein cholesterol (p ≤ 0.001, r = 0.70), high systolic blood pressure (p ≤ 0.001, r = 0.63), and high body mass index (p ≤ 0.001, r = 0.57), and DM2 (p ≤ 0.001, r = 0.38). The analysis results also illustrated a positive correlation between indoor air pollution and smoking (p ≤ 0.001, r = 0.92). HAP exposure might be a risk factor for elevated blood pressure, DM, obesity, and LDL cholesterol and, consequently, more serious health problems. According to our results, smoking is one of the sources of HAP. However, ecological studies cannot fully support causal relationships, and this article deals only with Iran. Our findings should be corroborated in personal exposure and biomonitoring approach studies.
Introduction
Household air pollution (HAP) is a main cause of death, with 3.8 million deaths annually1. Concentrations of HAP by significant human health effects2 in places such as the home, workplace, restaurants, and schools can be considered the most appropriate exposure measure in studies3,4. 95% of older people’s time is spent at home and indoors. Inadequate ventilation is a compelling dilemma in nursing homes5. In addition to the kinds of used fuel for cooking and the source of indoor heating energy, smoking, passive exposure to cigarette smoke and tobacco6, and outdoor air pollution can also be considered sources of indoor air pollution7. Some indoor air pollutants include radon, NOx, SO2, O3 (VOCs), PM, CO, and microorganisms7. Generally, air pollution can be inorganic, organic, biological, and radioactive8,9. Some pollutants, such as NOx, SO2, O3, and PM, are common indoors and outdoors. The concentrations of outdoor and indoor air pollutants are related to individual exposure to diverse environments10.
Recent studies showed a strong correlation between indoor air quality and smoking, cooking, and using fireplaces11. Cooking activities can increase the PM by about 1.5 to 27 times. In addition, there is some difference between the structure, chemical, and physical properties of indoor PM2.5 and outdoor PM2.5 and different health effects12. Due to the accumulation of pollutants, the absence of proper ventilation can severely affect residents’ health12. Some acute effects include eyes, noses, allergies, skin diseases, throat irritation, etc.13. Current studies have presented evidence of the association between increased death and long-term exposure to low concentrations of PM2.5 (< 30 μg/m3)14,15,16.
Because most patients are DM2, associations are shown mostly the effect of type 2. A Correlation between PM exposure and diabetes was shown in some studies17. Evidence of air pollution’s impact on diabetes is increasing, but most inquiries have been reported in high-income countries as the air pollution rate is high18,19. Short-term and long-term exposure to air pollution through the mechanism of inflammation, oxidative stress, and arterial regeneration can be associated with diastolic blood pressure (DBP) and systolic blood pressure (SBP)20,21. There is some report of a correlation between rising body mass index (BMI) and levels of PM2.5, PM10, NO2, NOx, and PM2.5 in the past literature22,23,24.
Forecasting Iran’s aging population will be 10.5% in 2025 and 21.7% in 2050, the oldest people in the region by 205025. Also, due to the high cost and the need for labor in indoor sampling, indoor air quality studies usually include information on a few homes that may not be well indicative of the exposure7. Therefore, considering the significance of indoor air pollution in the prevalence of adverse consequences of exposure, especially for the elderly, the present study intended to estimate the association between HAP and the majority of diabetes, hypertension, LDL cholesterol, and obesity in the Iranian population over 50 years, in 1990 to 2019 as an ecological study.
Materials and methods
Collecting data
Data were gathered separately from 1990 to 2019 based on sex and age groups 50–69 years and over 70 years, correlated to the prevalence of DM2, hypertension, and high BMI (body mass index). In addition, the death of risk factors, including tobacco use, smoking, drug use and alcohol use, was collected.
The data for systolic blood pressure (SBP) were measured in mmHg of 110 to 115 mmHg was used for TMREL SBP. For adults aged 20 and above, body mass index (BMI) is defined as greater than 20–25 kg/m2 of height. Diabetes mellitus is an example of a metabolic disease characterized by high glucose levels (hyperglycemia). The exposure to indoor air pollution was categorized based on the use of solid fuel for cooking, also known as HAP26. All data is collected from the official websites: http://www.healthdata.org/26.
According to the GBD 2019 study, this website presents injuries and risk factors from 1990 to 2019 in 204 countries. Finally, overall, 369 causes of illness and injury were systematically analyzed in this website. Details of the methodology and the main changes incorporated are described elsewhere27 and part of the data was also collected from the STEPS data based on the website https://vizit.tums.ac.ir/panel/steps-2020/en/main.html#/map.
Statistical analysis
After descriptive analysis, the Joinpoint regression model was used to show the trend status of the prevalence of DM2, in the Joinpoint software version 4.9.0.0. In addition, Annual Percent Change (APC) and Average Annual Percent Change (AAPC) were reported separately for men and women with their confidence intervals (CI). The significance level in all analyzes was 0.05.Another analyzes were performed using R software (version 3.5.0) using the Spearman correlation test. Interpretation of correlation relationship intensity was based on r = 0.8–1; very strong. r = 0.6–0.08; strong, r = 0.4–0.6; moderate, and r = 0.2–0.4; low or weak correlation relationship28. The maps were drawn using Datawrapper.
Results
Descriptive results of prevalence data
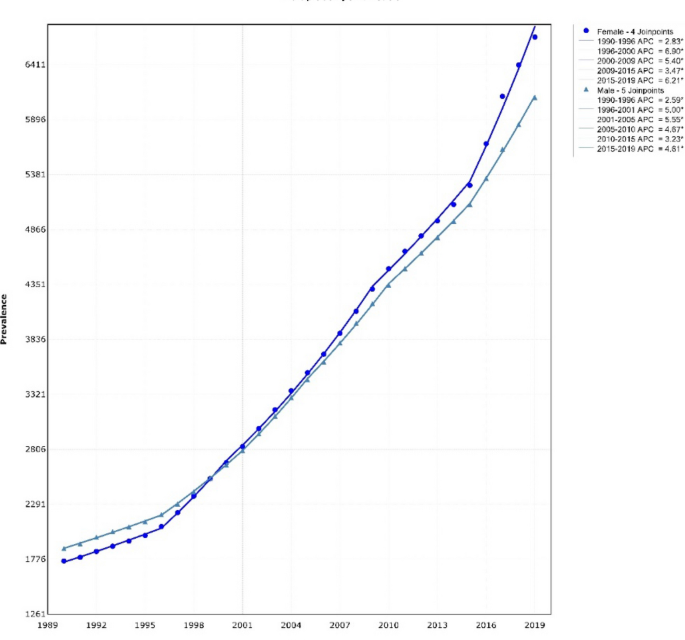
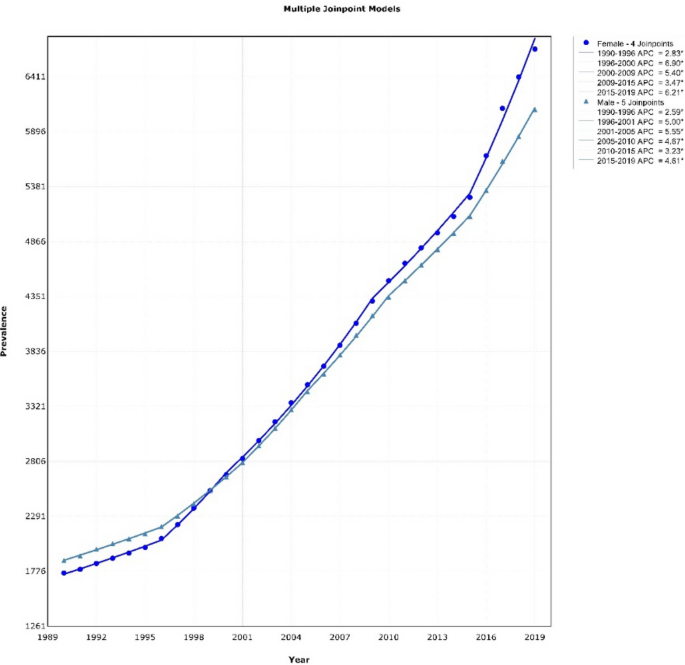
Descriptive results of the DM2 prevalence from 1990 to 2019 by gender in people over 50 years were shown in Fig. 1. These results indicated that the prevalence of DM2 in males had five joinpoints, and its general trend was upward [AAPC = 4.78% (CI 4.61–4.95)] and had four joinpoints in females, and the general trend was upward. [AAPC = 4.16% (CI 4.07–4.24)]. Descriptive results of DM2 prevalence also showed a strong upward trend in DM2 prevalence in women from 2015 to 2019 (APC = 6.21%). The descriptive results of the distribution of DM2 prevalence based on the HbA1c test, hypertension and obesity, by Iranian people 55–64, 65–74 and ≥ 75 years in 2020 (per 100,000) were shown in Fig. 2. For the age group of 55–64 years, the highest prevalence of DM2, hypertension and obesity were in Tehran, North Khorasan and Ardabil provinces, respectively. For the age group of 65–74 years, it was in Semnan, Hormozgan and Qom, respectively. For the age group over 75 years, it was in Khuzestan, Ardabil and Qom, respectively.
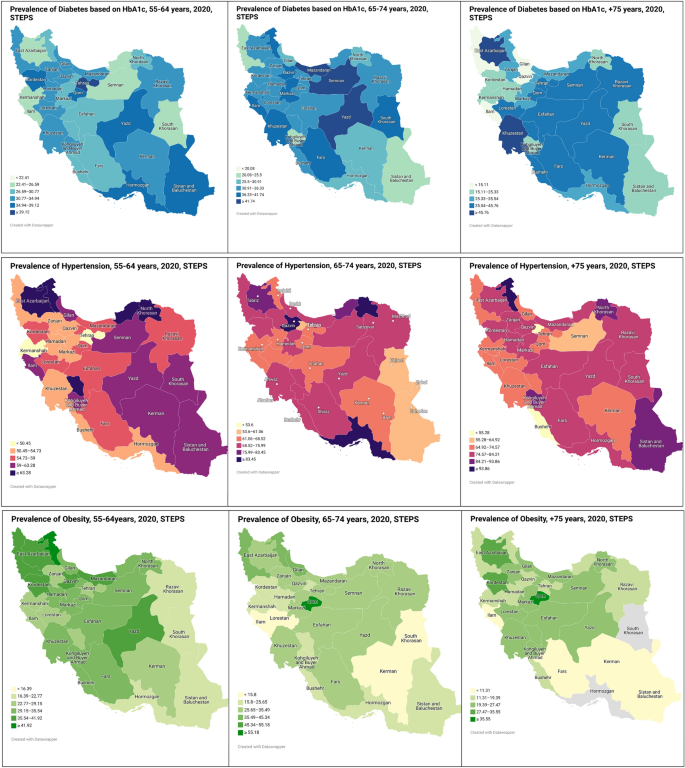
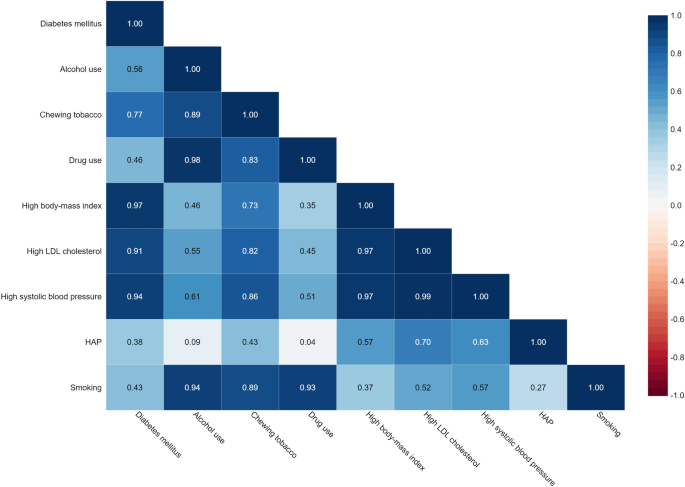
Indoor air pollution and prevalence of DM2, high SBP, obesity, and high LDL cholesterol
The related results between HAP exposure and the prevalence of DM2, high SBP, obesity, and high LDL cholesterol in the population over 50 years are shown in Fig. 3. A significant relationship positive correlation was discovered between HAP and DM2 prevalence (r = 0.38, p ≤ 0.001), high SBP (r = 0.63, p ≤ 0.001), high LDL cholesterol (r = 0.70, p ≤ 0.001) and high BMI (r = 0.57, p ≤ 0.001).
Correlation between the traditional risk factors and prevalence of DM2, high SBP, obesity, and high LDL cholesterol
The correlation between the prevalence of DM2, high SBP, obesity, and high LDL cholesterol in over 50 years population and the traditional risk factors for mentioned diseases, including smoking, drug use, alcohol consumption, and tobacco use was shown in Fig. 3. Correlation analysis results, significant relationship, and positive correlation were observed between smoking and prevalence of high SBP (r = 0.57, p ≤ 0.001), high LDL cholesterol levels (r = 0.52, p ≤ 0.001), high BMI (r = 0.37, p ≤ 0.001) and DM2 (r = 0.43, p ≤ 0.001). Correlation results showed a significant relationship positive correlation between tobacco use and prevalence of high SBP (r = 0.86, p ≤ 0.001), high levels of LDL cholesterol (r = 0.82, p ≤ 0.001), high BMI (r = 0.73, p ≤ 0.001), and DM2 (r = 0.77, p ≤ 0.001). Correlation analysis also showed a significant relationship positive correlation between alcohol consumption and prevalence of high SBP (r = 0.61, p ≤ 0.001), high levels of LDL cholesterol (r = 0.55, p ≤ 0.001), high BMI (r = 0.46, p ≤ 0.001), and DM2 (r = 0.56, p ≤ 0.001). In addition, Significant relationship positive correlation between drug use and high SBP prevalence (r = 0.51, p ≤ 0.001), high levels of LDL cholesterol (r = 0.45, p ≤ 0.001), high BMI (r = 0.97, p ≤ 0.001), and DM2 (r = 0.46, p ≤ 0.001) were the results of the correlation.
Relation between HAP and smoking, tobacco, and drug use
The correlation between HAP and smoking, tobacco, and drugs as risk factors for the mentioned disease are shown in Fig. 3. The results of Spearman correlation analysis showed a significant positive relationship between HAP and smoking (r = 0.92, p-Value ≤ 0.001). Therefore, according to the results of this study, smoking is one of the sources of HAP, an essential risk factor for DM2, high SBP, high levels of LDL cholesterol, and high BMI.
Discussion
About 3 billion people worldwide (especially in developing countries) have used fossil fuels for cooking and heating29. The association of HAP exposure with various diseases and premature death has been reported in previous studies30,31,32. It is estimated that approximately 2.8 million premature deaths worldwide result from exposure to HAP33. In summary, this study achieved two goals: (1) evaluating the situation of HAP exposure in Iran from 2000–2019, and (2) examining the correlation between HAP exposure and the prevalence of DM2, hypertension, obesity, and high LDL cholesterol in over 50 years old in Iran. The relationship between the mentioned disease’s prevalence and HAP exposure was investigated with risk factors such as smoking.
Incomplete combustion of solid fuels and tobacco use produces various pollutants such as CO, SO2, PM, carbon black (BC), toxic metals, and PAHs34,35,36, of which PM and PAH are important productions37,38. High emissions of indoor air pollutants may also be correlated with ambient air pollution39. Factors that are influenced by lifestyle in HAP exposure are the interior design of the kitchen, stove design, utilizing ventilation, cooking frequency, and passive smoking40. Rapid urbanization and industrialization have changed the structure of household energy consumption for cooking and heating41. According to Lee et al., living rooms and bedrooms must be separated from the kitchen. Living areas must be adequately ventilated to reduce exposure to air pollution40. Although in controlling air pollution, some ignore residential combustion compared to other sources of pollution, such as power plants and automobile emissions, HAP and its effects have raised growing concerns42.
Our study showed a significant relationship and positive correlation between HAP exposure and high SBP prevalence in the population aged 50 years and older in Iran. Several systematic studies have been conducted on HAP effects on health31,43,44. Exposure to indoor air pollutants can lead to absorption into the human body and accumulation in hair and lipid tissues45,46. PM inhalations have been outlined as a pathway for numerous metals to enter the body of humans47. Therefore, examining whether the metals uptake due to HAP exposure is related to blood pressure is necessary. Hypertension is considered the leading risk factor for heart disease globally, affecting more than one billion people globally, and 9.4 million new cases are recorded annually48. Besides some hypertension risk factors, including physical activity, smoking, and diet, environmental factors, notably air pollution, have been considered worldwide49,50. HAP Exposure caused by household solid fuel combustion is related to an increased risk of hypertension51. It increases the likelihood of detecting high BP in China52. Using biomass instead of liquefied petroleum gas increases particulate matter and the prevalence of hypertension53. HAP levels vary household by household and are challenging to monitor. Some inquiries reported the relationship between ambient air pollution and the risk of hypertension, but less research has been conducted about the association between HAP and the risk of hypertension. The results of our study illustrated a significant relationship and positive correlation between HAP exposure and DM2 prevalence in the population aged 50 years and older in Iran. DM2 is a conventional disease globally, and its prevalence has been rising in recent years54. Although obesity plays an important role in increasing DM2 prevalence, air pollution is also considered a potential risk factor for DM255,56. However, the effect of air pollution is not clearly described. The association between chronic exposure to air pollution, impaired glucose metabolism, development of insulin resistance, and the risk of DM2 has been assessed in several inquiries. However, this association is still unclear due to conflicting results57,58,59,60. Possible mechanisms include oxidative stress and persistent inflammation, with impaired insulin signaling, eventually leading to diabetes mellitus61.
This study’s correlation analysis shows a high BMI correlation and HAP exposure. Obesity is a chronic non-communicable disease associated with the risk of other diseases62. It has been observed that environmental stressors such as endocrine-disrupting chemicals can be responsible for obesity63,64. Air pollution is a risk factor for obesity caused by environmental factors65,66. Some animal studies showed air pollution could alter the body’s metabolism and contribute to weight gain67,68. In most of these reports, increasing BMI is associated with increased levels of NO2, NOx, PM2.5, PM10, and PM coarse23,69,70. Yang et al. conducted a study on people the age of 61 years old on average to examine the association between BMI and PM2.5, PM10, O3, CO, NO2, and SO2 in 125 Chinese cities. PM2.5 concentration for groups with BMI < 18.5, BMI = 18.5–23.9, BMI = 24–27.9, and BMI > 28 was reported 34.68 (mu)/m2, 36.12 (mu)/m2, 39.18 (mu)/m2, 41.07 (mu)/m2 respectively71. Also, Li et al. illustrated a positive impact of exposure to PM2.5 on BMI72.
The results of our study determined the relationship between HAP exposure and high LDL cholesterol in people over 50 years old in Iran. In this regard, Yang et al. (2018) study reported the association between PM2.5 and NO2 exposure and hypercholesterolemia by examining air pollution’s effect on fat levels and dyslipidemias. The results of Yang et al.’s (2018) research also illustrated that the association between air pollutants and dyslipidemias was more significant in participants who were overweight or obese73. Studies in rodents have also shown that exposure to PM2.5 comprises an inflammatory response in visceral adipose tissue74,75 or epidermal adipose tissue76.
This study demonstrated a significant relationship between smoking and HAP, although the results indicate a weak correlation between smoking and HAP. In our study, smoking also showed a moderate correlation with DM2 prevalence, high systolic BP, high LDL cholesterol, and obesity. Smoking is a severe concern for public health globally. Many healthcare planners try to design and implement appropriate strategies to decrease smoking as the most critical factor related to mortality77,78. Smoking prevalence is relatively high in Iran79. Literature also reported smoking had been considered an important source of HAP7,80. Our study results are adopted with the previous research on smoking and even exposure to secondhand smoke (a risk factor for hypertension)21, diabetes81, obesity82, and high LDL cholesterol83.
Strengths and limitations
A global study of disease burden has estimated that HAP is liable for more than 3 million premature deaths worldwide and is the fourth most common risk factor for all deaths32. This research analyzed the relationship between exposure to HAP and common chronic diseases, especially in the elderly. In addition, we showed the relationship between exposure to HAP and traditional risk factors for the prevalence of these diseases. Previous studies have focused on the relationship between people’s health and occupational and environmental exposures. In many cases, measuring an individual’s long-term exposure to air pollutants requires a lot of time and money. We were able to solve this problem mainly by using an ecological study84. However, any research has its limitations. This study was done as an ecological study, and in fact, the results of our study were from a data set85. Generalizing the results to all people will lead us to ecological fallacies. They are considering that ambient air pollution and the cumulative impacts of air pollutants can also potentially impact the prevalence of these diseases. Various factors such as fuel and stove types, burning frequency, people characteristics, ventilation conditions, the structure of the room, different seasons, fuel/energy types, environmental and meteorological conditions, and other sources of pollution as critical factors can affect indoor air pollution86. However, limited information has been reported on these influential factors. Identifying key factors and perceptions of how indoor air quality changes is essential to designing an efficient solution to boost air quality.
Suggestion
Reducing individual exposure to indoor air pollutants, especially in vulnerable populations including diabetics, people with high LDL cholesterol, high BP, and high BMI, can be done through simple measures, such as the installation of ventilation systems with filtration for houses in polluted areas, especially for people at risk, proper use of primary or secondary contraceptives to counteract the potential effects of HAP exposure87. The preferred method for assessing personal exposure to air pollutants is portable personal samplers with a high ability to estimate daily inhalation exposure. In addition to CO, SO2, and PM, exposure assessment of most air pollutants is necessary to arrange a more reliable interpretation of the health effects of exposed individuals. Investigating the source of HAP with different resource allocation methods for various pollutants can also be considered in future studies. Assessing the health consequences of HAP exposure according to the investigation of particular biomarkers and epidemiological inquiries is essential. These studies increase our knowledge of the detrimental effects of HAP and assist in assuring the public and policymakers of more severe proceedings for this issue.
Conclusion
This inquiry is the first ecological study on exposure to indoor air pollution and the prevalence of chronic diseases in the age group over 50. This study illustrated a positive relationship between HAP exposure and the prevalence of DM2, high SBP, obesity, and high LDL cholesterol in the population over 50 years in Iran. In addition, smoking was shown to be a source of HAP and a risk factor for the diseases listed. This study was ecological and focused only on the elderly in Iran. Causal relationships cannot be fully supported through ecological studies. Fuel is one of the most important factors effective in HAP and exposure. Moreover, ventilation conditions significantly affect air quality. This issue is expected to be explored in future studies. To investigate the health effects of indoor air pollution, we use vulnerable older populations because they spend more of their time at home than others; the need for future studies with personal sampling is significantly felt. Health professionals play an essential part in supporting educational and policy initiatives as well as advising their patients.
Data availability
All used raw data in this study are available at http://www.healthdata.org/. The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
References
-
No Title. https://www.who.int/respiratory/copd/en/.
-
Noonan, C. W., Ward, T. J., Navidi, W. & Sheppard, L. A rural community intervention targeting biomass combustion sources: Effects on air quality and reporting of children’s respiratory outcomes. Occup. Environ. Med. 69, 354–360 (2012).
-
Ohura, T., Amagai, T., Senga, Y. & Fusaya, M. Organic air pollutants inside and outside residences in Shimizu, Japan: Levels, sources and risks. Sci. Total Environ. 366, 485–499 (2006).
-
Adgate, J. L., Ramachandran, G., Pratt, G. C., Waller, L. A. & Sexton, K. Spatial and temporal variability in outdoor, indoor, and personal PM2.5 exposure. Atmos. Environ. 36, 3255–3265 (2002).
-
Almeida-Silva, M., Wolterbeek, H. T. & Almeida, S. M. Elderly exposure to indoor air pollutants. Atmos. Environ. 85, 54–63 (2014).
-
Li, Z., Wen, Q. & Zhang, R. Sources, health effects and control strategies of indoor fine particulate matter (PM2.5): A review. Sci. Total Environ. 586, 610–622 (2017).
-
Yeatts, K. B. et al. Indoor air pollutants and health in the United Arab Emirates. Environ. Health Perspect. 120, 687–694 (2012).
-
Leung, D. Y. C. Outdoor-indoor air pollution in urban environment: Challenges and opportunity. Front. Environ. Sci. 2, 69 (2015).
-
Tolabi, Z. et al. The investigation of type and concentration of bio-aerosols in the air of surgical rooms: A case study in Shariati hospital, Karaj. MethodsX 6, 641–650 (2019).
-
Johnson, M. et al. Modeling approaches and performance for estimating personal exposure to household air pollution: A case study in Kenya. Indoor Air https://doi.org/10.1111/ina.12790 (2021).
-
Habre, R. et al. Sources of indoor air pollution in New York City residences of asthmatic children. J. Expo. Sci. Environ. Epidemiol. 24, 269–278 (2014).
-
Bruce, N. et al. WHO indoor air quality guidelines on household fuel combustion: Strategy implications of new evidence on interventions and exposure–risk functions. Atmos. Environ. 106, 451–457 (2015).
-
Ghaffarianhoseini, A. et al. Sick building syndrome: Are we doing enough?. Archit. Sci. Rev. 61, 99–121 (2018).
-
Crouse, D. L. et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: A Canadian national-level cohort study. Environ. Health Perspect. 120, 708–714 (2012).
-
Hart, J. E. et al. The association of long-term exposure to PM 2.5 on all-cause mortality in the Nurses’ Health Study and the impact of measurement-error correction. Environ. Heal. 14, 1–9 (2015).
-
Ji, W. & Zhao, B. Estimating mortality derived from indoor exposure to particles of outdoor origin. PLoS ONE 10, e0124238 (2015).
-
Rajagopalan, S. & Brook, R. D. Air pollution and type 2 diabetes: Mechanistic insights. Diabetes 61, 3037–3045 (2012).
-
Wang, B. et al. Mechanisms in endocrinology: Effect of long-term exposure to air pollution on type 2 diabetes mellitus risk: A systemic review and meta-analysis of cohort studies. Eur. J. Endocrinol. 171, R173–R182 (2014).
-
Lucht, S. A. et al. Air pollution and glucose metabolism: An analysis in non-diabetic participants of the Heinz Nixdorf recall study. Environ. Health Perspect. 126, 47001 (2018).
-
Brook, R. D. et al. Differences in blood pressure and vascular responses associated with ambient fine particulate matter exposures measured at the personal versus community level. Occup. Environ. Med. 68, 224–230 (2011).
-
Baumgartner, J. et al. Indoor air pollution and blood pressure in adult women living in rural China. Environ. Health Perspect. 119, 1390–1395 (2011).
-
de Bont, J. et al. Ambient air pollution and overweight and obesity in school-aged children in Barcelona. Spain. Environ. Int. 125, 58–64 (2019).
-
Dong, G.-H. et al. Interactions between air pollution and obesity on blood pressure and hypertension in Chinese children. Epidemiology 26, 740–747 (2015).
-
McConnell, R. et al. A longitudinal cohort study of body mass index and childhood exposure to secondhand tobacco smoke and air pollution: The Southern California Children’s Health Study. Environ. Health Perspect. 123, 360–366 (2015).
-
Noroozian, M. The elderly population in Iran: An ever growing concern in the health system. Iran. J. Psychiatry Behav. Sci. 6, 1 (2012).
-
Dicker, D. et al. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1684–1735 (2018).
-
Miller, D. C. & Salkind, N. J. Handbook of Research Design and Social Measurement (Sage, 2002).
-
Bonjour, S. et al. Solid fuel use for household cooking: Country and regional estimates for 1980–2010. Environ. Health Perspect. 121, 784–790 (2013).
-
Clark, M. L. et al. Health and household air pollution from solid fuel use: The need for improved exposure assessment. Environ. Health Perspect. 121, 1120–1128 (2013).
-
Zhang, J. & Smith, K. R. Household air pollution from coal and biomass fuels in China: Measurements, health impacts, and interventions. Environ. Health Perspect. 115, 848–855 (2007).
-
Lim, S. S. et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2224–2260 (2012).
-
Cohen, A. J. et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 389, 1907–1918 (2017).
-
Massey, D. D., Habil, M. & Taneja, A. Particles in different indoor microenvironments-its implications on occupants. Build. Environ. 106, 237–244 (2016).
-
O’Connor, R. J. et al. Toxic metal and nicotine content of cigarettes sold in China, 2009 and 2012. Tob. Control 24, iv55–iv59 (2015).
-
Shen, G. et al. Field measurement of emission factors of PM, EC, OC, parent, nitro-, and oxy-polycyclic aromatic hydrocarbons for residential briquette, coal cake, and wood in rural Shanxi, China. Environ. Sci. Technol. 47, 2998–3005 (2013).
-
Wang, B. et al. Human bronchial epithelial cell injuries induced by fine particulate matter from sandstorm and non-sandstorm periods: Association with particle constituents. J. Environ. Sci. 47, 201–210 (2016).
-
Wang, B. et al. Properties and inflammatory effects of various size fractions of ambient particulate matter from Beijing on A549 and J774A. 1 cells. Environ. Sci. Technol. 47, 10583–10590 (2013).
-
Chafe, Z. A. et al. Household cooking with solid fuels contributes to ambient PM2.5 air pollution and the burden of disease. Environ. Health Perspect. 122, 1314–1320 (2014).
-
Li, Z. et al. Indoor air pollution from coal combustion and the risk of neural tube defects in a rural population in Shanxi Province, China. Am. J. Epidemiol. 174, 451–458 (2011).
-
Massey, D. D., Kulshrestha, A. & Taneja, A. Particulate matter concentrations and their related metal toxicity in rural residential environment of semi-arid region of India. Atmos. Environ. 67, 278–286 (2013).
-
Liu, Q. & Liu, L. The effects of daily fuels combustion on indoor air quality in rural area of northern Anhui province. J. Environ. Heal. 28, 702–705 (2011).
-
Mehta, S., Shin, H., Burnett, R., North, T. & Cohen, A. J. Ambient particulate air pollution and acute lower respiratory infections: A systematic review and implications for estimating the global burden of disease. Air Qual. Atmos. Heal. 6, 69–83 (2013).
-
Kim, K.-H., Jahan, S. A. & Kabir, E. A review of diseases associated with household air pollution due to the use of biomass fuels. J. Hazard. Mater. 192, 425–431 (2011).
-
Schummer, C., Appenzeller, B. M. R., Millet, M. & Wennig, R. Determination of hydroxylated metabolites of polycyclic aromatic hydrocarbons in human hair by gas chromatography–negative chemical ionization mass spectrometry. J. Chromatogr. A 1216, 6012–6019 (2009).
-
Pereira, R., Ribeiro, R. & Goncalves, F. Scalp hair analysis as a tool in assessing human exposure to heavy metals (S. Domingos mine, Portugal). Sci. Total Environ. 327, 81–92 (2004).
-
Zheng, N., Liu, J., Wang, Q. & Liang, Z. Health risk assessment of heavy metal exposure to street dust in the zinc smelting district, Northeast of China. Sci. Total Environ. 408, 726–733 (2010).
-
Organization, W. H. A global brief on hypertension: silent killer, global public health crisis: World Health Day 2013. (2013).
-
Liu, C. et al. Ambient particulate air pollution and daily mortality in 652 cities. N. Engl. J. Med. 381, 705–715 (2019).
-
Giorgini, P. et al. Air pollution exposure and blood pressure: An updated review of the literature. Curr. Pharm. Des. 22, 28–51 (2016).
-
Mohapatra, I., Das, S. C. & Samantaray, S. Health impact on women using solid cooking fuels in rural area of Cuttack district, Odisha. J. Fam. Med. Prim. Care 7, 11 (2018).
-
Qiu, Y., Yang, F.-A. & Lai, W. The impact of indoor air pollution on health outcomes and cognitive abilities: Empirical evidence from China. Popul. Environ. 40, 388–410 (2019).
-
Dutta, A., Mukherjee, B., Das, D., Banerjee, A. & Ray, M. R. Hypertension with elevated levels of oxidized low-density lipoprotein and anticardiolipin antibody in the circulation of premenopausal Indian women chronically exposed to biomass smoke during cooking. Indoor Air 21, 165–176 (2011).
-
Liu, J. et al. Trends in the incidence of diabetes mellitus: results from the Global Burden of Disease Study 2017 and implications for diabetes mellitus prevention. BMC Public Health 20, 1–12 (2020).
-
Nolan, C. J., Damm, P. & Prentki, M. Type 2 diabetes across generations: From pathophysiology to prevention and management. Lancet 378, 169–181 (2011).
-
Polonsky, K. S. The past 200 years in diabetes. N. Engl. J. Med. 367, 1332–1340 (2012).
-
Coogan, P. F. et al. Air pollution and incidence of hypertension and diabetes mellitus in black women living in Los Angeles. Circulation 125, 767–772 (2012).
-
Andersen, Z. J. et al. Diabetes incidence and long-term exposure to air pollution: A cohort study. Diabetes Care 35, 92–98 (2012).
-
Brook, R. D. et al. Long-term fine particulate matter exposure and mortality from diabetes in Canada. Diabetes Care 36, 3313–3320 (2013).
-
Chen, H. et al. Risk of incident diabetes in relation to long-term exposure to fine particulate matter in Ontario, Canada. Environ. Health Perspect. 121, 804–810 (2013).
-
Liu, C. et al. Exaggerated effects of particulate matter air pollution in genetic type II diabetes mellitus. Part. Fibre Toxicol. 11, 1–14 (2014).
-
Simkova, S., Veleminsky, M. & Sram, R. J. The impact of air pollution to obesity. Neuroendocrinol. Lett. 41, 146–153 (2020).
-
Schug, T. T., Janesick, A., Blumberg, B. & Heindel, J. J. Endocrine disrupting chemicals and disease susceptibility. J. Steroid Biochem. Mol. Biol. 127, 204–215 (2011).
-
Nasab, H., Mirzaee, M., Hashemi, M. & Rajabi, S. Measurement of urinary triclocarban and 2, 4-dichlorophenol concentration and their relationship with obesity and predictors of cardiovascular diseases among children and adolescents in Kerman, Iran. J. Environ. Public Health 2022, 1–9 (2022).
-
Hashemi, M., Rajabi, S., Eghbalian, M., Suliburska, J. & Nasab, H. Demographic and anthropometric characteristics and their effect on the concentration of heavy metals (arsenic, lead, chromium, zinc) in children and adolescents. Heliyon 9, e13621 (2023).
-
McConnell, R. et al. Does near-roadway air pollution contribute to childhood obesity?. Pediatr. Obes. 11, 1 (2016).
-
Bolton, J. L. et al. Prenatal air pollution exposure induces neuroinflammation and predisposes offspring to weight gain in adulthood in a sex-specific manner. FASEB J. 26, 4743–4754 (2012).
-
Sun, Q. et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation 119, 538–546 (2009).
-
Jerrett, M. et al. Traffic-related air pollution and obesity formation in children: A longitudinal, multilevel analysis. Environ. Heal. 13, 49 (2014).
-
Mejía, J. F., Choy, S. L., Mengersen, K. & Morawska, L. Methodology for assessing exposure and impacts of air pollutants in school children: Data collection, analysis and health effects–a literature review. Atmos. Environ. 45, 813–823 (2011).
-
Yang, Z., Song, Q., Li, J. & Zhang, Y. Air pollution as a cause of obesity: Micro-level evidence from Chinese cities. Int. J. Environ. Res. Public Health 16, 4296 (2019).
-
Li, M. et al. Sex-specific difference of the association between ambient air pollution and the prevalence of obesity in Chinese adults from a high pollution range area: 33 communities Chinese health study. Atmos. Environ. 117, 227–233 (2015).
-
Yang, B.-Y. et al. Exposure to ambient air pollution and blood lipids in adults: The 33 communities Chinese Health Study. Environ. Int. 119, 485–492 (2018).
-
de Melo, J. O. et al. Inhalation of fine particulate matter during pregnancy increased IL-4 cytokine levels in the fetal portion of the placenta. Toxicol. Lett. 232, 475–480 (2015).
-
Xu, X. et al. Effect of early particulate air pollution exposure on obesity in mice: Role of p47phox. Arterioscler. Thromb. Vasc. Biol. 30, 2518–2527 (2010).
-
Wei, Y. et al. Chronic exposure to air pollution particles increases the risk of obesity and metabolic syndrome: Findings from a natural experiment in Beijing. FASEB J. 30, 2115–2122 (2016).
-
Allen, S. I. et al. Peer reviewed: Tobacco use among middle and high school students in Pennsylvania. Prev. Chronic Dis. https://doi.org/10.5888/pcd15.170289 (2018).
-
Rudatsikira, E., Muula, A. S. & Siziya, S. Current cigarette smoking among in-school American youth: Results from the 2004 National Youth Tobacco Survey. Int. J. Equity Health 8, 1–9 (2009).
-
Ebrahimi, H., Sahebihagh, M. H., Ghofranipour, F., Mohammadpoorasl, A. & Tabrizi, J. Cigarette smoking patterns in adult smokers of Iran A content analysis study. Nurs. Midwifery J. 13, 1104–1118 (2016).
-
Li, N. et al. Effects of passive smoking on hypertension in rural Chinese nonsmoking women. J. Hypertens. 33, 2210–2214 (2015).
-
Chang, S. A. Smoking and type 2 diabetes mellitus. Diabetes Metab. J. 36, 399–403 (2012).
-
Dare, S., Mackay, D. F. & Pell, J. P. Relationship between smoking and obesity: A cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS ONE 10, e0123579 (2015).
-
Gepner, A. D. et al. Effects of smoking and smoking cessation on lipids and lipoproteins: Outcomes from a randomized clinical trial. Am. Heart J. 161, 145–151 (2011).
-
Dehghani, S. et al. Ecological study of ambient air pollution exposure and mortality of cardiovascular diseases in elderly. Sci. Rep. 12, 21295 (2022).
-
Vali, M. et al. Effect of meteorological factors and Air Quality Index on the COVID-19 epidemiological characteristics: An ecological study among 210 countries. Environ. Sci. Pollut. Res. 28, 1–11 (2021).
-
Du, W., Li, X., Chen, Y. & Shen, G. Household air pollution and personal exposure to air pollutants in rural China—A review. Environ. Pollut. 237, 625–638 (2018).
-
De Hartog, J. J., Boogaard, H., Nijland, H. & Hoek, G. Do the health benefits of cycling outweigh the risks?. Environ. Health Perspect. 118, 1109–1116 (2010).
Acknowledgements
The authors would like to appreciate all the subjects who participated in the study.
Author information
Authors and Affiliations
Contributions
S.D.: Conceptualization, Methodology, Investigation, Writing. S.Y.: Writing- Reviewing and Editing. V.O.: Writing- Reviewing and Edit. M.T.: Reviewing and Editing. Mohammad S.M.: Reviewing and Editing. M.S.: Reviewing and Editing. M.V.: Supervision, Resources, Validation, Conceptualization. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dehghani, S., Yousefi, S., Oskoei, V. et al. Ecological study on household air pollution exposure and prevalent chronic disease in the elderly.
Sci Rep 13, 11763 (2023). https://doi.org/10.1038/s41598-023-39059-9
-
Received:
-
Accepted:
-
Published:
-
DOI: https://doi.org/10.1038/s41598-023-39059-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.