Faisal-Cury A, Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Women Ment Health. 2007;10(1):25–32.
Previti G, Pawlby S, Chowdhury S, Aguglia E, Pariante CM. Neurodevelopmental outcome for offspring of women treated for antenatal depression: a systematic review. Arch Women Ment Health. 2014;17(6):471–83.
Fekadu Dadi A, Miller ER, Mwanri L. Antenatal depression and its association with adverse birth outcomes in low and middle-income countries: a systematic review and meta-analysis. PLoS ONE. 2020;15(1):e0227323.
Field T. Prenatal depression effects on early development: a review. Infant Behav Dev. 2011;34(1):1–14.
Sakowicz A, Allen E, Alvarado-Goldberg M, Grobman WA, Miller ES. Association between Antenatal Depression Symptom Trajectories and Preterm Birth. Obstet Gynecol. 2023;141(4):810–7.
Zanardo V, Sandri A, Straface G. Trajectories of antenatal depression and increased odds of preterm birth. Am J Obstet Gynecol. 2022;226(2):278.
Toscano M, Royzer R, Castillo D, Li D, Poleshuck E. Prevalence of depression or anxiety during Antepartum Hospitalizations for Obstetric Complications: a systematic review and Meta-analysis. Obstet Gynecol. 2021;137(5):881–91.
Bernard NK, Bogat GA, Kashy DA, Lonstein JS, Levendosky AA. Prenatal and postnatal intimate partner violence, depression, and infant-mother touch. Infant Behav Dev. 2022;67:101703.
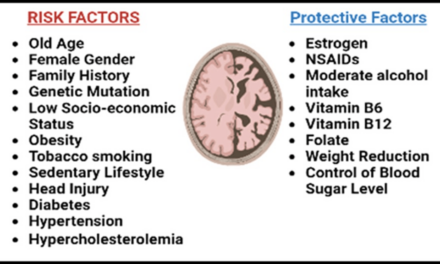
Leigh B, Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry. 2008;8:24.
McCoy SJ, Beal JM, Shipman SB, Payton ME, Watson GH. Risk factors for postpartum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature. J Am Osteopath Assoc. 2006;106(4):193–8.
Zhang L, Wang L, Cui S, Yuan Q, Huang C, Zhou X. Prenatal depression in women in the third trimester: prevalence, predictive factors, and Relationship with maternal-fetal attachment. Front Public Health. 2020;8:602005.
Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202(1):5–14.
Kalmbach DA. The emerging role of prenatal insomnia therapy in the prevention of perinatal depression and anxiety. Sleep 2022, 45(5).
Sedov ID, Anderson NJ, Dhillon AK, Tomfohr-Madsen LM. Insomnia symptoms during pregnancy: a meta-analysis. J Sleep Res. 2021;30(1):e13207.
Gupta R, Rawat VS. Sleep and sleep disorders in pregnancy. Handb Clin Neurol. 2020;172:169–86.
Sivertsen B, Hysing M, Dorheim SK, Eberhard-Gran M. Trajectories of maternal sleep problems before and after childbirth: a longitudinal population-based study. BMC Pregnancy Childbirth. 2015;15:129.
Mindell JA, Cook RA, Nikolovski J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. 2015;16(4):483–8.
Facco FL, Chan M, Patel SR. Common Sleep Disorders in pregnancy. Obstet Gynecol. 2022;140(2):321–39.
Yu Y, Li M, Pu L, Wang S, Wu J, Ruan L, Jiang S, Wang Z, Jiang W. Sleep was associated with depression and anxiety status during pregnancy: a prospective longitudinal study. Arch Women Ment Health. 2017;20(5):695–701.
Tham EK, Tan J, Chong YS, Kwek K, Saw SM, Teoh OH, Goh DY, Meaney MJ, Broekman BF. Associations between poor subjective prenatal sleep quality and postnatal depression and anxiety symptoms. J Affect Disord. 2016;202:91–4.
Plancoulaine S, Flori S, Bat-Pitault F, Patural H, Lin JS, Franco P. Sleep trajectories among pregnant women and the impact on outcomes: a Population-Based Cohort Study. Matern Child Health J. 2017;21(5):1139–46.
Wang G, Deng Y, Jiang Y, Lin Q, Dong S, Song Y, Zhu L, Zhu Q, Sun W, Zhang Y et al. Trajectories of sleep quality from late pregnancy to 36 months postpartum and association with maternal mood disturbances: a longitudinal and prospective cohort study. Sleep 2018, 41(12).
Emamian F, Khazaie H, Okun ML, Tahmasian M, Sepehry AA. Link between insomnia and perinatal depressive symptoms: a meta-analysis. J Sleep Res. 2019;28(6):e12858.
Wolynczyk-Gmaj D, Majewska A, Bramorska A, Rozanska-Waledziak A, Ziemka S, Brzezicka A, Gmaj B, Czajkowski K, Wojnar M. Cognitive Function Decline in the Third Trimester of Pregnancy Is Associated with Sleep Fragmentation. J Clin Med 2022, 11(19).
Alhola P, Polo-Kantola P. Sleep deprivation: impact on cognitive performance. Neuropsychiatr Dis Treat. 2007;3(5):553–67.
Tucker AM, Whitney P, Belenky G, Hinson JM, Van Dongen HP. Effects of sleep deprivation on dissociated components of executive functioning. Sleep. 2010;33(1):47–57.
Skurvydas A, Zlibinaite L, Solianik R, Brazaitis M, Valanciene D, Baranauskiene N, Majauskiene D, Mickeviciene D, Venckunas T, Kamandulis S. One night of sleep deprivation impairs executive function but does not affect psychomotor or motor performance. Biol Sport. 2020;37(1):7–14.
McSorley VE, Bin YS, Lauderdale DS. Associations of sleep characteristics with cognitive function and decline among older adults. Am J Epidemiol. 2019;188(6):1066–75.
Nuno L, Gomez-Benito J, Carmona VR, Pino O. A systematic review of executive function and information Processing Speed in Major Depression Disorder. Brain Sci 2021, 11(2).
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Tsai PS, Wang SY, Wang MY, Su CT, Yang TT, Huang CJ, Fang SC. Psychometric evaluation of the chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual life research: Int J Qual life aspects Treat care rehabilitation. 2005;14(8):1943–52.
Dietch JR, Taylor DJ, Sethi K, Kelly K, Bramoweth AD, Roane BM. Psychometric evaluation of the PSQI in U.S. College Students. J Clin Sleep Med. 2016;12(8):1121–9.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J psychiatry: J mental Sci. 1987;150:782–6.
Joshi U, Lyngdoh T, Shidhaye R. Validation of hindi version of Edinburgh postnatal depression scale as a screening tool for antenatal depression. Asian J Psychiatr. 2020;48:101919.
Kozinszky Z, Dudas RB. Validation studies of the Edinburgh postnatal depression scale for the antenatal period. J Affect Disord. 2015;176:95–105.
Stewart RC, Umar E, Tomenson B, Creed F. Validation of screening tools for antenatal depression in Malawi–a comparison of the Edinburgh postnatal depression scale and self reporting questionnaire. J Affect Disord. 2013;150(3):1041–7.
Zhao Y, Kane I, Wang J, Shen B, Luo J, Shi S. Combined use of the postpartum depression screening scale (PDSS) and Edinburgh postnatal depression scale (EPDS) to identify antenatal depression among chinese pregnant women with obstetric complications. Psychiatry Res. 2015;226(1):113–9.
Wang Y, Guo X, Lau Y, Chan KS, Yin L, Chen J. Psychometric evaluation of the Mainland Chinese version of the Edinburgh postnatal depression scale. Int J Nurs Stud. 2009;46(6):813–23.
Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evid report/technology Assess 2005(119):1–8.
Jensen AR, Rohwer WD Jr. The Stroop color-word test: a review. Acta Psychol. 1966;25(1):36–93.
Hayes AF, Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. Br J Math Stat Psychol. 2014;67(3):451–70.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY, US: Guilford Press; 2013.
Ananth CV. Proportion mediated in a causal mediation analysis: how useful is this measure? BJOG: an international journal of obstetrics and gynaecology. 2019;126(8):983.
Okun ML, Kiewra K, Luther JF, Wisniewski SR, Wisner KL. Sleep disturbances in depressed and nondepressed pregnant women. Depress Anxiety. 2011;28(8):676–85.
Hung HM, Tsai PS, Ko SH, Chen CH. Patterns and predictors of sleep quality in taiwanese pregnant women. MCN The American journal of maternal child nursing. 2013;38(2):95–101.
Kalmbach DA, Cheng P, Ong JC, Ciesla JA, Kingsberg SA, Sangha R, Swanson LM, O’Brien LM, Roth T, Drake CL. Depression and suicidal ideation in pregnancy: exploring relationships with insomnia, short sleep, and nocturnal rumination. Sleep Med. 2020;65:62–73.
Polo-Kantola P, Aukia L, Karlsson H, Karlsson L, Paavonen EJ. Sleep quality during pregnancy: associations with depressive and anxiety symptoms. Acta Obstet Gynecol Scand. 2017;96(2):198–206.
Chee MW, Chuah LY, Venkatraman V, Chan WY, Philip P, Dinges DF. Functional imaging of working memory following normal sleep and after 24 and 35 h of sleep deprivation: correlations of fronto-parietal activation with performance. NeuroImage. 2006;31(1):419–28.
Duman RS, Aghajanian GK. Synaptic dysfunction in depression: potential therapeutic targets. Science. 2012;338(6103):68–72.
Duman RS, Aghajanian GK, Sanacora G, Krystal JH. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(3):238–49.
Disner SG, Beevers CG, Haigh EA, Beck AT. Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci. 2011;12(8):467–77.
Joormann J, Gotlib IH. Emotion regulation in depression: relation to cognitive inhibition. Cogn Emot. 2010;24(2):281–98.
Szelenberger W, Niemcewicz S. Event-related current density in primary insomnia. Acta Neurobiol Exp (Wars). 2001;61(4):299–308.
Varkevisser M, Kerkhof GA. Chronic insomnia and performance in a 24-h constant routine study. J Sleep Res. 2005;14(1):49–59.
Roiser JP, Elliott R, Sahakian BJ. Cognitive mechanisms of treatment in depression. Neuropsychopharmacology. 2012;37(1):117–36.
Rock PL, Roiser JP, Riedel WJ, Blackwell AD. Cognitive impairment in depression: a systematic review and meta-analysis. Psychol Med. 2014;44(10):2029–40.
Halahakoon DC, Lewis G, Roiser JP. Cognitive impairment and Depression-Cause, Consequence, or coincidence? Jama Psychiat. 2019;76(3):239–40.
Lim J, Dinges DF. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychol Bull. 2010;136(3):375–89.
Jin X, Ye E, Qi J, Wang L, Lei Y, Chen P, Mi G, Zou F, Shao Y, Yang Z. Recovery sleep reverses impaired response inhibition due to Sleep Restriction: evidence from a visual event related potentials study. PLoS ONE. 2015;10(12):e0142361.
Chung KF, Lee CT, Yeung WF, Chan MS, Chung EW, Lin WL. Sleep hygiene education as a treatment of insomnia: a systematic review and meta-analysis. Fam Pract. 2018;35(4):365–75.
Yu SH, Tseng CY, Lin WL. A Neurofeedback Protocol for executive function to reduce Depression and Rumination: a controlled study. Clin Psychopharmacol Neurosci. 2020;18(3):375–85.