Amid the recent uptick in COVID hospitalizations, a new round of vaccines is being introduced. The shots could be particularly important for Black Americans, who have continued to show an increased risk for severe complications from the virus.
Although much smaller than past spikes, COVID deaths have risen above 1,000 per week this month and hospitalizations have risen above 20,000 a week, according to the Centers for Disease Control and Prevention. Why are we seeing more cases? It might be because more people sought indoor shelter during a summer of record heat, kids are back in classrooms, and community immunity from previous infections and vaccines is waning over time.
Black Americans have been harder hit by the spike than the general population. This reflects somewhat lower vaccination rates and the decreased likelihood of being prescribed antiviral medications, like Paxlovid, that prevent serious complications. Higher prevalence of underlying conditions like heart disease, diabetes, and high blood pressure also continue to be a factor.
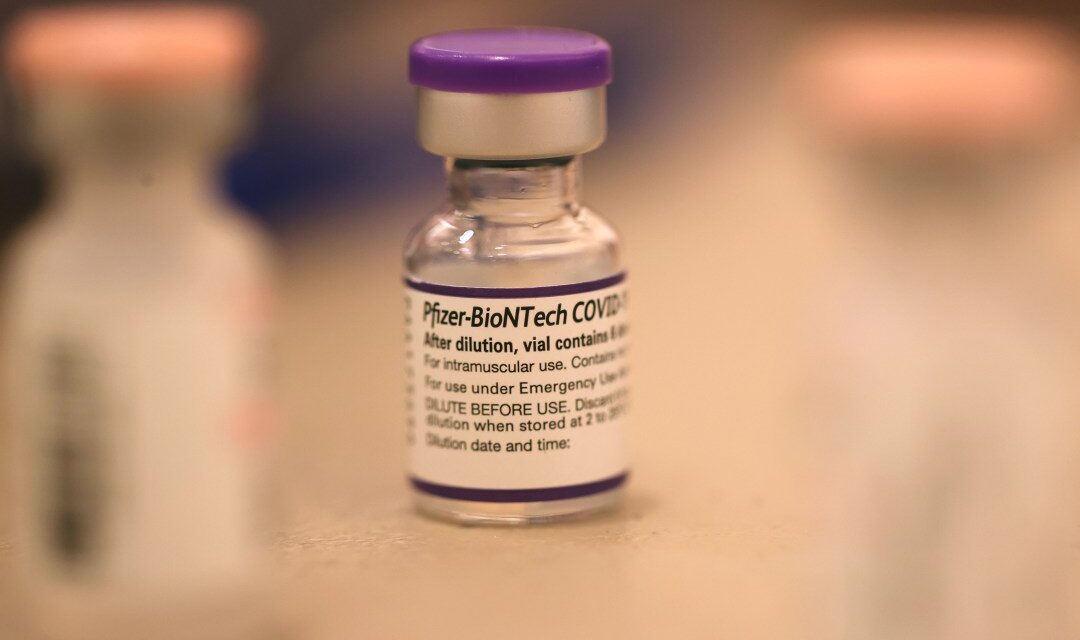
Some businesses, schools, and hospitals have reinstated mask mandates in recent weeks, and the Biden administration recently restarted distribution of free COVID-19 tests. Rollout of the latest vaccines began this month after the U.S. Food and Drug Administration approved the new Pfizer and Moderna shots.
Here’s what you should know about the coronavirus as we head into fall:
Who should get an updated vaccine?
The CDC recommends COVID vaccination for everyone over the age of 6 months. Because Black folks have higher rates of underlying health conditions, the vaccine is an added layer of protection.
“These are the individuals who really need to have these vaccinations,” said Dr. Dial Hewlett, the chair of the COVID vaccine and therapeutics committee at the National Medical Association.
In Westchester County, New York, where Hewlett works, they’ve administered the vaccine to both infants around 6 months old and to older residents. Both groups have tolerated the vaccine well, he said.
If I’ve had previous shots and/or been infected with COVID-19 in the past, should I still consider this vaccine?
Yes, you are still at risk of infection if you’ve had COVID before or were previously vaccinated.
“We know that immunity to COVID wanes, so it wears off over time — whether it be immunity that someone acquired through an infection or through a vaccine,” said Dr. Oni Blackstock, a primary care and HIV physician in New York.
Also, the updated COVID vaccines were developed based on an Omicron subvariant called XBB.1.5, which is one of the more common variants circulating now. The vaccines from Moderna and Pfizer are effective and equally safe. While not 100% effective at preventing infection, both are very effective at preventing serious illness and long COVID, the varied symptoms — including respiratory problems, chest pain, and fatigue — that have lingered in some people for weeks or years after their initial infection.
How can I get the shot? How much does it cost?
The Bridge Access Program, a $1 billion effort through the Department of Health and Human Services, is providing free vaccines for uninsured and underinsured individuals at pharmacies across the country. These free vaccines can be accessed at CVS and Walgreens, as well as local health departments and federally qualified health centers.
For those with commercial insurance, many plans won’t require a copay, so there should be no cost. However, some people have run up against roadblocks, including some pharmacies running out of doses and insured patients being told they have to pay out of pocket for the shot, which can retail for up to $200 with an administration fee. The Department of Health and Human Services said it is working to smooth out the difficulties.
It’s unclear when exactly those hiccups will clear up, but checking with your local health department, pharmacy, or primary care physicians to see when vaccines will be readily available is a good first step, doctors say. You can also visit vaccines.gov to find a location near you.
Flu season is coming up. Can I get both vaccines at the same time?
Yes, you can get COVID and flu shots simultaneously. It’s safe, Blackstock said, and might be the most time effective option for many. Unlike the flu, the coronavirus is not a seasonal virus, which means new variants can pop up and spread at any time of the year.
Throughout the coronavirus pandemic, there were disparities in who got vaccinated, with Black folks being left behind. That changed, however, with outreach and education from grassroots organizations as well as local and federal health officials.
“That has kind of fallen off, particularly with the booster,” Blackstock said, leaving Black people less likely to have the most updated shot. Black Americans tend to have low rates of flu vaccination, as well.
“It’s equally important to get the flu vaccine,” Hewlett said. “It is also very important for our pregnant women, our future mothers, to be vaccinated,” as it can prevent infections for newborns in the first few months of birth.
What do we know about the most recent number of COVID-19 cases, hospitalizations, and deaths?
A lot of the widespread measurement and data reporting tools implemented in earlier phases of the pandemic, like weekly case number reports and pop-up testing sites, have been discontinued. So much of what we know about how the virus is spreading now is based on hospitalization data and levels of the virus in wastewater. The exact case number is unknown.
“We don’t have a way to report if you’re positive or negative at home,” said Dr. Deshira Wallace, an assistant professor at the University of North Carolina Chapel Hill’s Gillings School of Global Public Health. “We don’t know how many people actually have COVID.”
The latest CDC data shows an uptick in hospitalizations. This mini surge is much lower than what we saw before the initial round of COVID-19 vaccines in 2020 or during the Omnicron wave in 2021. There’s also been an increase in wastewater levels, however that measure does not fully capture the extent to which the virus is circulating because it might not be available in every city or in rural areas.
“We don’t have a lot of data available,” said Dr. Oni Blackstock, a primary care and HIV physician in New York. “When there’s no data, it feels like there’s no problem.”
Over the course of the pandemic, Black Americans’ rate of dying from the virus was about double that of white people, and they are nearly three times as likely to be hospitalized, according to CDC data. Vaccines, community immunity from prior infections and the availability of antiviral medications is likely a protective factor against a spike in hospitalizations and death like what we saw in 2020.
“We’re all very happy that we’re not where we were in 2020 and 2021,” said Hewlett. Still, he said, “we don’t want to become complacent.”
Capital B is a nonprofit news organization dedicated to uncovering important stories — like this one — about how Black people experience America today. As more and more important information disappears behind paywalls, it’s crucial that we keep our journalism accessible and free for all. But we can’t publish pieces like this without your help. If you support our mission, please consider becoming a member by making a tax-deductible donation. Thank you!