Introduction
Pain assessments are a routine part of health screening in healthcare systems like the Veterans Health Administration (VHA).1 However, previous studies have not assessed whether pain screening varies for sexual and gender minority persons, which includes individuals who identify as lesbian, gay, bisexual, and/or transgender (LGBT). Even fewer studies have addressed differences in pain among LGBT Veterans. An understanding of the epidemiology of pain in the growing population of LGBT Veterans will be essential as the VHA plans pain treatment services.
It is important to understand how pain may be experienced or manifest differently by people with different lived experiences to better address pain. Experiences of discrimination, stigma, and prejudice (ie, minority stress2), may lead patients to delay seeking care, which may exacerbate pain.3–6 For example, transgender Veterans may encounter discrimination from medical professionals.3,4 Hughto et al found 27% of transgender individuals experienced stigma in a healthcare setting, and stigma was strongly associated with both opioid pain medication misuse and unmet healthcare needs.4 Zajacova et al found bisexual and transgender/queer+ individuals were substantially more likely to report pain, dissatisfaction with healthcare, and sought care outside the healthcare system.7 Not surprisingly, some LGBTQ individuals who experience discrimination and unmet chronic pain management adopt maladaptive coping mechanisms such as substance use that lead to poorer health outcomes.8,9
Furthermore, experience of pain was found to be associated with elevated risk of suicide and suicidal ideation.10 Knowing the prevalence as well as the severity of pain in LGBT populations may enhance the VHA’s ability to care for at-risk Veterans.11
We sought to evaluate pain screening, pain intensity, and persistent pain among LGBT Veterans in comparison with those who did not have data that would classify them as LGBT based on our methods, which for brevity we refer to as non-LGBT Veterans. We hypothesized that LGBT Veterans would have more overall pain than non-LGBT Veterans, and among those who reported pain, they would have more persistent pain than non-LGBT Veterans.
Methods
Study Design and Sample
Using data from the Corporate Data Warehouse, a national repository of data of over 9 million Veterans in care that contains all clinical, administrative, laboratory, and pharmacy data for every Veteran in the VHA nationwide, patients were classified as LGBT or non-LGBT from Fiscal year (FY) 2010 to 2019 (ie, October 1, 2010 to September 30, 2019), using natural language processing.12,13 Fifteen established key terms (Lesbian, Gay, Bisexual, Transgender, Trans woman, Transwoman, Trans man, Transman, Cisgender, Homosexual, LGBT, LGBTQ, LGBTQI, Queer, and Intersex) were used to capture LGBT status.12 The natural language processing method had 88.2% sensitivity and 91.5% specificity to identify LGBT status.12 All VHA patients with one or more visits to primary care, defined by clinic stop codes (27, 301, 310, 318, 319, 322, 323, 348, 350, and 404), in the observation period were eligible, and the cohort entry (ie, enrollment date) was the first primary care visit. The LGBT cohort was established to examine suicide because minority stress (eg, discrimination) associated with being a sexual or gender minority within the VA may increase risk of suicide. This current study takes a cross-sectional look to examine pain within this sample.
Setting
Veterans Health Administration, the largest integrated healthcare system in the United States of patients 18 years old and older, was the study setting.
Outcome
The outcome of interest was self-reported pain intensity numeric rating score (NRS) that ranges from 0 to 10,14,15 where 0 is no pain and 10 is the worst possible pain. If multiple scores were taken on the same day, the highest score would be retained. We looked at 3 outcomes related to pain scores assessed within 1 year of enrollment: 1) screened for pain (yes/no), 2) pain intensity (0–10), and 3) persistent pain (yes/no), defined as three or more scores ≥4 in at least three months (among those who had three or more monthly pain scores available).16 Due to an excess of zeroes in the pain intensity scores, the scores were modeled in two ways: one model for any pain, defined as score ≥1 (yes/no), and another model for pain score among those with any pain.
Primary Predictor
LGBT status (LGBT vs non-LGBT) derived from VHA records was the predictor of interest.
Covariates
Covariates included potential confounders of the relationship between LGBT status and pain, such as demographics: sex recorded in the VHA electronic health records, which is assumed to be sex recorded at birth; age; race and/or ethnicity; relationship status; mental health: post-traumatic stress disorder (PTSD) and major depression; substance use: alcohol and/or drug use disorders; musculoskeletal disorder (MSD); and number of clinic visits within 1 year of enrollment.
Age was at time of cohort entry and was categorized in 10-year increments from <25 up to>
Statistical Analysis
Descriptive analysis of this retrospective cross-sectional cohort looked at patients’ characteristics overall and by LGBT classification using a t-test for continuous variables and chi-square for categorical variables. Recognizing the potential differential experience of gender minority persons (eg, transgender) compared to sexual minorities (lesbian, gay, bisexual), descriptive analyses were re-ran comparing LGB vs non-LGBT vs transgender Veterans.
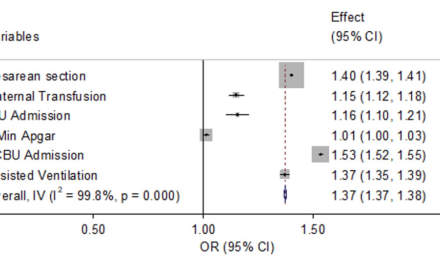
We used a robust Poisson regression model17,18 with a log link and robust variance estimates to calculate relative risks (RR) and 95% confidence intervals (CI) to examine the association between LGBT Veterans (yes/no) and binary outcomes of pain: screening, any pain, and persistent pain. This method was employed because our study was a cohort study design, and the primary outcomes were common events. We used a truncated negative binomial model for the pain score among those with any pain (ie, scores ≥ 1). Models for any pain were re-ran stratified by LGB, non-LGBT, and transgender Veterans. All models were adjusted for demographics, mental health, substance use, MSD, and number of clinic visits.
Ethical Approval
Our study was approved by the institutional review board (IRB) of the Veterans Affairs Connecticut Healthcare System (IRB# 1583220). It has been granted a waiver of informed consent and is compliant with the Health Insurance Portability and Accountability Act (HIPAA).
The analytic data sets used for this study are confidential and protected behind the VA firewall and cannot be accessed without a data use agreement. No further data will be shared besides those already reported. For more information, please visit https://www.virec.research.va.gov or contact the VA Information Resource Center at [email protected]. Statistical analyses were conducted with SAS, version 9.4.
Results
There were 1,149,486 Veterans in the study sample, of which 218,154 (19%) classified as LGBT. The mean age of patients was 52 years old. LGBT Veterans were more likely to be younger (ie, age < 65), recorded female, Black or Hispanic, never married, and have one or more of the following diagnoses: musculoskeletal disorder, mental illness, and/or substance use. LGBT Veterans also had more recorded clinic visits (Table 1). In addition, LGBT Veterans were more likely to be screened for pain compared to non-LGBT Veterans (94% vs 89%) and slightly more likely to report persistent pain (39% vs 37%).
|
Table 1 Patient Characteristics Overall and by LGBT Classification |
Overall, 55% (N = 628,813) of study patients had 3 or more monthly pain scores available. LGBT Veterans were more likely to have 3 or more monthly pain scores documented: 65% (N = 141,705) in the LGBT group vs 52% (N = 487,108) in the non-LGBT group.
Across all classifications, transgender Veterans were more likely to be younger, recorded female, divorced/other, have a diagnose of PTSD or major depression, and have higher pain scores. They were also more likely to report moderate (transgender Veterans 21% vs 19% for both LGB and non-LGBT Veterans) to severe pain (transgender Veterans 18% vs 16% for both LGB and non-LGBT Veterans) and persistent pain (transgender Veterans 42% vs 38% for LGB and 37% for non-LGBT Veterans) (Table 2).
|
Table 2 Patient Characteristics Overall and by Lesbian, Gay, or Bisexual (LGB), Transgender, and Non-LGBT |
In regression models adjusted for covariates, LGBT Veterans’ likelihood of being screened for pain, compared to non-LGBT Veterans, was 2.5% higher (95% CI 2.3%, 2.6%) (Table 3). Other factors associated with getting screened for pain included a mental health diagnosis, MSD, and older age (Table 3). Among those screened for pain, the risk of any pain was 2.1% lower (95% CI 1.6%, 2.6%) for LGBT Veterans. A diagnosis of alcohol use disorder was also associated with lower pain among those screened (Table 3).
|
Table 3 Factors Associated with 1) Pain Screening, 2) Any Pain, and 3) Persistent Pain |
For persistent pain, the model indicated that there was no significant difference between LGBT and non-LGBT Veterans in terms of persistent pain (RR = 1.00, 95% CI (0.99, 1.01), p = 0.88), after adjusting for covariates (Table 3). Younger Veterans were more likely to have persistent pain relative to Veterans 75 and older (for example, Veterans 45–55 years old compared to those 75 and older were 79% more likely to report persistent pain). Black Veterans were 12% more likely to report persistent pain compared to White Veterans. The risk for persistent pain was 15% higher for those divorced/other versus never married, 20% higher for those with drug use disorder (versus not), and 25% higher for those with PTSD (versus not). MSD had the strongest association with persistent pain (RR = 3.65, 95% CI (3.60, 3.69), p < 0.001).
In the model looking at the pain score (among those with any pain) as a count variable (truncated negative binomial), we found similar results. The mean pain score for LGBT Veterans was slightly (1%) lower compared to non-LGBT Veterans (Table 4). In contrast to the results in the model looking at any pain as a binary outcome, Black and Hispanic Veterans had significantly higher pain than White Veterans, and being married and <25 years old were no longer significant predictors in the model looking at pain score>
|
Table 4 Model of the Pain Score as a Count Variable (Truncated Negative Binomial) Among Those with Any Pain |
In stratified models, results were largely similar across LGB, non-LGBT, and transgender groups regarding factors associated with pain (Table 5). Younger Veterans were more likely to report pain than those 75 and older. For example, Veterans <25>
|
Table 5 Factors Associated with Any Pain Stratified by Lesbian, Gay, or Bisexual (LGB), Transgender, and Non-LGBT |
Discussion
In a diverse nationwide sample, LGBT Veterans were more likely to be screened for pain. Among those who reported any pain, LGBT Veterans were more likely to have lower pain scores (albeit these differences were relatively small), and no difference in regard to persistent pain. Notably, transgender Veterans on average were more likely to have greater and more persistent pain, and for those with a diagnosis of drug use disorder versus those without a diagnosis of drug use disorder there was a 3% higher reporting of any pain.
Reasons for more frequent pain screening among LGBT Veterans cannot be determined from our study. More frequent pain screening could be a result of patient-initiated identification of pain, for example. More research is needed to identify the reasons for frequency of pain screening among LGBT Veterans compared to heterosexual, cisgender counterparts.
Past research has begun to unpack complex relationships among sexual orientation, gender identity, culture, experiences of discrimination, and pain.19 A recent study showed that type and level of hormones can play a role in pain perception and experience: persons with estrogen exposure have greater and higher temporomandibular disorders, fibromyalgia and visceral pain, while the drop in estrogen among those recorded female at birth at menopause intensifies musculoskeletal pain.20 Furthermore, higher substance use rates among LGBT Veterans, which aligns with past research,21 may reflect self-medicating to alleviate pain, thus potentially underestimating pain scores among this population (see Table 4). This potential interaction between LGBT status, substance use, and pain is serious and warrants further exploration. Additionally, areas of resiliency among LGBT Veterans to mitigate decades of targeted marketing from alcohol and tobacco industries and encourage healthier forms of coping warrant further and urgent exploration.
Our study aligns with past research indicating that transgender persons often report greater pain scores for a variety of reasons, including postoperative pain.22 In our study, LGBT persons had more documented clinic visits. However, it is important to note that healthcare seeking behaviors can vary widely among LGBT persons, so future research should disaggregate subpopulations within the LGBT community when reporting clinic visit frequency. Investigation of reasons for healthcare seeking and avoidance is warranted.3 The association of drug use disorder among transgender patients in this study may be an indication of self-medication perhaps due to poor pain care. Additionally, while not the primary study question, the significantly higher pain scores (Table 4) and more persistent pain (Table 3) among Black Veterans is a serious and important finding that should be addressed by the VHA. These findings may be a result of minority stress and/or poor pain management. It is well established that Black individuals are differentially assessed and treated for pain due to systematic and structural biases,23 and in a recent study examining disparity in chronic pain, sexual minority adults experienced substantially significantly more pain than their straight counterparts, potentially due to upstream stigmatization.7
Limitations to this study include the necessarily subjective nature of pain scores—some individuals might underreport pain in order to avoid attention, and some may report pain more frequently for complex reasons. It is also crucial to point out the variability of safely disclosing LGBT status among diverse geopolitical locations in the US and the earned mistrust of the medical system on the part of LGBT people and LGBT Veterans in particular. Workman et al found variation in LGBT terminology and prevalence by time and geography12 which suggests access, provider knowledge, and affirming care is not universal. Of note, LGBT status was ascertained through natural language processing, and misclassification is possible. Although this method had high sensitivity and specificity, it did not allow for identification of sexual orientation for transgender Veterans and gender identity for LGB Veterans.12 LGB and non-LGB Veterans could not be confirmed as cisgender given limitations of current data collection. Furthermore, the proportion of Veterans classified as LGBT are among those who had sexual orientation or gender identity information recorded, and there may be a bias in who is being asked about sexual orientation or gender identity and who is not. A more systematic way of identifying LGBT status is needed, and the VHA has already made strides to improve data collection for sexual orientation.24 We were also limited to sex recorded in the VHA electronic health records which was either male or female, an imperfect and often inaccurate proxy of anatomy and gender. The VHA added gender identity options to the medical record in 2017 and this became available to all users in 2022. Veterans can also enter their gender identity online through VA.GOV (Alexis Matza, personal communication, May 1, 2023). Work using these more inclusive gender options is needed. Finally, the large sample size may show statistically significant differences that are not clinically meaningful.
Conclusion
Our study provides a novel examination of frequency of pain screening and pain experiences among Veterans stratified by LGBT status. Our study cannot make conclusions on the reasons for frequency of pain screening nor reasons for pain experienced by Veterans of diverse sexual orientations and genders. It is notable that transgender and Black Veterans reported the greatest pain. Additional research is needed to examine level of comfort of disclosure of LGBT status as well as drivers of pain screening and pain scores in the VHA.
Acknowledgments
Any expressed views do not represent those of the US Government, Department of Veterans Affairs.
Author Contributions
Drs. Gordon and Buta had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Gordon and Buta were responsible for study concept and design, interpretation, and critical revisions. Drs. Gordon, Buta and Pratt-Chapman were instrumental in drafting the manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by VA HSR&D IIR 18-035 (Zeng and Goulet, PI’s).
Disclosure
Dr T Elizabeth Workman reports grants from US Department of Veterans Affairs, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Pain as the 5 Th Vital Sign Toolkit [Internet]; 2000. Available from: https://www.va.gov/painmanagement/docs/toolkit.pdf.
2. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi:10.1037/0033-2909.129.5.674
3. Pratt-Chapman ML, Murphy J, Hines D, et al. ”When the pain is so acute or if I think that I’m going to die”: health care seeking behaviors and experiences of transgender and gender diverse people in an urban area. PLoS One. 2021;16(2):e0246883. doi:10.1371/journal.pone.0246883
4. Hughto JMW, Restar AJ, Wolfe HL, et al. Opioid pain medication misuse, concomitant substance misuse, and the unmet behavioral health treatment needs of transgender and gender diverse adults. Drug Alcohol Depend. 2021;222:108674. doi:10.1016/j.drugalcdep.2021.108674
5. Hutchinson MK, Thompson AC, Cederbaum JA. Multisystem factors contributing to disparities in preventive health care among lesbian women. J Obstet Gynecol Neonatal Nurs. 2006;35(3):393–402. doi:10.1111/j.1552-6909.2006.00054.x
6. Molina Y, Lehavot K, Beadnell B, et al. Racial disparities in health behaviors and conditions among lesbian and bisexual women: the role of internalized stigma. LGBT Health. 2014;1(2):131–139. doi:10.1089/lgbt.2013.0007
7. Zajacova A, Grol-Prokopczyk H, Liu H, Reczek R, Nahin RL. Chronic pain among U.S. sexual minority adults who identify as gay, lesbian, bisexual, or “something else”. Pain. 2023;164(9):1942–1953. doi:10.1097/j.pain.0000000000002891
8. Reisner SL, Pardo ST, Gamarel KE, White Hughto JM, Pardee DJ, Keo-Meier CL. Substance use to cope with stigma in healthcare among U.S. Female-to-Male Trans Masculine Adults. LGBT Health. 2015;2(4):324–332. doi:10.1089/lgbt.2015.0001
9. Abd-Elsayed A, Heyer AM, Schatman ME. Disparities in the treatment of the LGBTQ population in chronic pain management. J Pain Res. 2021;14:3623–3625. doi:10.2147/JPR.S348525
10. Racine M. Chronic pain and suicide risk: a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):269–280. doi:10.1016/j.pnpbp.2017.08.020
11. Kessler RC, Bauer MS, Bishop TM, et al. Using administrative data to predict suicide after psychiatric hospitalization in the Veterans Health Administration System. Front Psychiatry. 2020;11(390). doi:10.3389/fpsyt.2020.00390
12. Workman TE, Goulet JL, Brandt CA, et al. Temporal and geographic patterns of documentation of sexual orientation and gender identity keywords in clinical notes. Med Care. 2023;61(3):130–136. doi:10.1097/MLR.0000000000001803
13. Blosnich JR, Cashy J, Gordon AJ, et al. Using clinician text notes in electronic medical record data to validate transgender-related diagnosis codes. J Am Med Inform Assoc. 2018;25(7):905–908. doi:10.1093/jamia/ocy022
14. McCaffery M, Beebe A. Pain: Clinical Manual for Nursing Practice. Mosby St. Louis, MO: Mosby Incorporated; 1989.
15. McCaffery M, Beebe A. The Numeric Pain Rating Scale Instructions. In: Pain: Clinic Manual for Nursing Practice; 1989.
16. Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330(9):592–596. doi:10.1056/NEJM199403033300902
17. Goulet JL, Buta E, Bathulapalli H, et al. Statistical models for the analysis of zero-inflated pain intensity numeric rating scale data. J Pain. 2017;18(3):340–348. doi:10.1016/j.jpain.2016.11.008
18. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi:10.1093/aje/kwh090
19. Wallace B, Varcoe C, Holmes C, et al. Towards health equity for people experiencing chronic pain and social marginalization. Int J Equity Health. 2021;20(1):53. doi:10.1186/s12939-021-01394-6
20. Athnaiel O, Cantillo S, Paredes S, et al. The role of sex hormones in pain-related conditions. Int J Mol Sci. 2023;24(3):1866. doi:10.3390/ijms24031866
21. Anderson-Carpenter KD, Rutledge JD, Mitchell K. Prescription opioid misuse among heterosexual versus lesbian, gay, and bisexual military Veterans: evidence from the 2015–2017 national survey of drug use and health. Drug Alcohol Depend. 2020;207:107794. doi:10.1016/j.drugalcdep.2019.107794
22. Ferrando CA, Chapman G, Pollard R. Preoperative pain symptoms and the incidence of endometriosis in transgender men undergoing hysterectomy for gender affirmation. J Minim Invasive Gynecol. 2021;28(9):1579–1584. doi:10.1016/j.jmig.2021.01.018
23. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between Blacks and Whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–4301. doi:10.1073/pnas.1516047113
24. Department of Veterans Affairs, Veterans Health Administration. Provision of Health Care for Veterans Who Identify as Lesbian, Gay, Bisexual and Queer: VHA Directive 1340. Washington, DC; 2022.